Because patients in intensive care units (ICUs) are, by definition, in dire health, the consequences of even the slightest medical error can be devastating.
Two quality-improvement studies by researchers at Washington University School of Medicine in St Louis suggest solutions to two of the most common and dangerous patient safety challenges in this population: restoring normal phosphorus levels and preventing infections caused by catheters. The studies resulted in dramatic improvements.
The research was a multi-disciplinary effort between physicians, nurses, dietitians and the rest of the surgical ICU team at Barnes-Jewish Hospital. The team believes these initiatives should be applicable to any ICU in the country.
“Unlike anything else in the ICU, there’s no risk involved in implementing these initiatives, and the only cost is the small amount of time it takes to train the medical staff,” says lead investigator Craig M. Coopersmith, M.D. “The ICU depends on a multidisciplinary team approach, and everyone wants to do what’s best for the patient. Our efforts were very well received by the entire team, and we’re extremely pleased with the results.”
The studies were published in the February 2004 issues of the Journal of the American College of Surgeons and the journal Archives of Surgery. At the beginning of April, Coopersmith, an associate professor of surgery and assistant professor of anesthesiology, also presented the findings at the 24th International Symposium on Intensive Care and Emergency Medicine in Brussels, Belgium.
Freedom from phosphorus problems
About one-quarter of all ICU patients have abnormally low levels of the chemical phosphorus in their body. The condition, called hypophosphatemia, can damage nearly every system in the body, and patients with this condition have more than twice the risk of death as those with normal phosphorus levels. To date, even the most successful efforts to restore phosphorus levels have only a 50 percent chance of working. In severe cases, the chance of success falls to 30 percent.
“Nobody knows a good way to restore normal phosphorus levels,” Coopersmith explains. “Until now, none of the published studies that have tested ways to improve the situation have worked.”

Together with dietitian Beth E. Taylor, Coopersmith developed a new algorithm to determine how much phosphorus treatment to provide to any given patient. By incorporating the patient’s weight, potassium levels and the severity of hypophosphatemia, the algorithm provides a consistent and clear-cut way of determining the best course of treatment.
The results were dramatic. Before implementing the new protocol, the ICU’s success rates with phosphorus treatment were similar to the national average: 53 percent success in patients with moderate hypophosphatemia, 27 percent in severe cases. After training the ICU staff and implementing the new procedure, success rates jumped to 78 percent in moderate hypophosphatemia and 63 percent in severe cases. Overall, the success of treatment increased from 47 percent to 76 percent.
“We were shocked at how profound our results were, ” Coopersmith says.
The researchers also were surprised by something else: When evaluating baseline success rates of treatment before implementing the new protocol, they discovered two types of medical errors. First, some patients with hypophosphatemia were not treated for the condition; second, some patients with normal phosphorus levels were treated as though they had abnormal levels.
After implementing the new treatment protocol, the percentage of hypophosphatemic patients who were not treated for the condition dropped from 26 percent to 11 percent. The number of patients with normal phosphorus levels who were inappropriately treated plummeted from 51 percent to 16 percent.
“Helping decrease the prevalence of errors was a very nice bonus that we didn’t expect,” Coopersmith says. “Clearly just encouraging the team to pay attention to this problem made a difference. This also shows that in the increasingly complex world of ICU medicine, developing definitive protocols can help.”
Keeping catheters clean
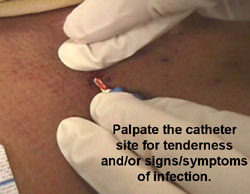
Central venous catheters — plastic tubes threaded through the main blood vessels that lead to and from the heart — are ubiquitous in the ICU. Physicians rely on them to deliver nutrients and drugs directly into the bloodstream and to monitor levels of a variety of biological markers.
But because these tubes are exposed to the outside world, they can provide an opening for bacteria to enter the body, making patients particularly vulnerable to infection. As many as 35 percent of catheter-related bloodstream infections are fatal.
“We always have to walk the fine line between helping a patient and putting them at risk for infection,” Coopersmith says. “As with everything we do, we know using central venous catheters is necessary and beneficial but may inadvertently harm some patients.”
Because of the risk, many hospitals track the number of infections in the ICU and submit their findings to a national database called the National Nosocomial Infections Surveillance (NNIS) system, run by the Centers for Disease Control and Prevention.
Between January 1998 and June 1999, Coopersmith’s group reported infection rates that were almost double the national average, so his team developed an educational program to address the problem. After distributing educational packets and a 20-question multiple-choice examination to the ICU staff, the group reexamined infection rates over the next 18 months. The number dropped from twice to about half the national average.
“The program is very simple, yet it had extremely dramatic effects,” Coopersmith says. “We’ve literally had requests from all over the country and the world for information on how to implement this type of initiative.”
Coopersmith and his colleagues were thrilled with the improvements, but they weren’t completely satisfied.
“Although our rates were down to half the national average, they weren’t down to zero,” he explains. “The goal is to have no infections at all.”
To determine how to improve the situation even more, the team secretly evaluated the placement and maintenance of central venous catheters for 15 months. They found that some behaviors had improved, but others had not.
Coopersmith says the findings are encouraging.
“Clearly the educational program had an effect,” he explains. “But the fact that some mistakes were still made means there still are things we can do to improve even further.”
His team therefore decided to implement a behavioral intervention. Whereas the first initiative focused on education, the second round focused on behaviors. They broke down catheter placement and maintenance procedures into discrete steps and placed manuals and guidelines throughout the ICU. They also informed the staff of their findings and pointed out specific areas of weakness.
Fifteen months into this behavioral intervention, the infection rate had again decreased. During that same time period, the national average increased.
“This study has several major implications,” Coopersmith says. “The first lesson is that educational interventions are productive, but they do not necessarily result in behavioral changes. The second lesson is that even if you have a successful program you probably can do better. The more we pay attention to these issues, the more patients will benefit.”
Taylor BE, Huey WY, Buchman TG, Boyle WA, Coopersmith CM. Treatment of hypophosphatemia using a protocol based on patient weight and serum phosphorus level in a surgical intensive care unit. Journal of the American College of Surgeons, vol. 198(2), pp. 198-204, February 2004.
Coopersmith CM, Zack JE, Ward MR, Sona CS, Schallom ME, Everett SJ, Huey WY, Garrison TM, McDonald J, Buchman TG, Boyle WA, Fraser VJ, Polish LB. The impact of bedside behavior on catheter-related bacteremeia in the intensive care unit. Archives of Surgery, vol. 139(2), pp. 131-136, February 2004.
This research was supported by the Centeres for Disease Control and Prevention, the BJC Hospital Epidemiology and Infection Control Consortium and the National Institutes of Health.
The full-time and volunteer faculty of Washington University School of Medicine are the physicians and surgeons of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Recognizing its excellence in nursing care, Barnes-Jewish Hospital is the first adult hospital in the state of Missouri to be certified as a “Magnet Hospital” by the American Nurses Credentialing Center (ANCC). The Magnet Award is the highest honor awarded for hospital nursing by the ANCC.