The bacterium responsible for strep throat, scarlet fever and other disorders appears to use a single wasplike “stinger” to spread infection, according to surprised microbiologists at Washington University School of Medicine in St. Louis.
Researchers studying the surface of Streptococcus pyogenes, also known as Strep A, had expected to find a disordered jumble of several pumps for spraying compounds onto cells targeted for infection. Instead, they found a single dedicated stinger — a feature Strep A may share with other bacteria that could provide an easier target for new drugs designed to treat infections.
“It’s certainly a long time down the road, but this gives us new ways to think about how strep and other bacteria might one day be stopped,” says Michael G. Caparon, Ph.D., professor of molecular microbiology and the study’s lead investigator. “With better understanding of how bacteria interact with the cells they infect, we can start to develop better approaches for intervening.”
Strep A is one of the most common human pathogens. Epidemiologists estimate that at any given time 5 to 15 percent of humans carry asymptomatic Strep A in their respiratory tracts. Strep bacteria has become increasingly more resistant to antibiotic drugs during the last decade, and serious infection by the bacteria can produce a “flesh-eating” condition called necrotizing fasciitis.
On the basis of the Strep A’s outer membrane, microbiologists classify it as a Gram-positive bacteria. Gram-positive bacteria only have one outer membrane, but Gram-negative bacteria have two outer membranes separated by a small space.
That space between the inner and outer membranes serves as a prep room for proteins and other agents that Gram-negative bacteria secrete to infect host cells. Many proteins won’t function properly unless they have folded into a particular configuration, and scientists believe the space between the two membranes provides Gram-negative bacteria with a place to ensure the right folding and other preparatory steps take place.
Caparon was curious about how Gram-positive bacteria like Strep A prepare their infectious agents without this airlock-like space between membranes.
“Strep A is known to secrete more than 30 different substances as a part of its infectious processes,” he says. “Some are toxins, some interact with host cell receptors and make the cells die or behave differently. We wanted to know how does Strep A emits these agents: Is it organized in any fashion, or does it just happen randomly?”

Most microbiological evidence had suggested the latter hypothesis might be a better bet. Bacteria seemed to have little structural organization beyond the shape of the cells they came in, which can vary from round to cigar to corkscrew shapes. But a few studies, including some from Caparon’s lab, recently had begun to hint that Strep A bacteria might be more organized than scientists suspected.
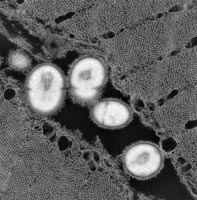
For the study, Caparon and graduate student Jason Rosch used modified antibodies to tag an infectious agent secreted by Strep A. They then took micrographs of the bacteria. The antibodies consistently showed up at a single focal point where the cell was secreting the infectious agent.
After follow-up tests confirmed that what they had observed was not a byproduct of the experiment’s design, Caparon decided to name the new structure that secretes infectious agents. He calls it the “exportal,” a combination of export and portal.
“We’d like to now look at how the cell actually puts this together,” Caparon says. “If we can identify the factors that actually are involved in structurally putting the exportal together, those may be the most interesting points of intervention for devising new drug treatments.”
Caparon also wants to test other Gram-positive bacteria to learn if they have exportals, too.
Rosch J, and Caparon M. A microdomain for protein secretion in Gram-positive bacteria. Science, June 4, 2004, 1513-1515.
Funding from the National Institutes of Health.
The full-time and volunteer faculty of Washington University School of Medicine are the physicians and surgeons of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked second in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.