To remain healthy, all cells must quickly mend any breaks that arise in their DNA strands. But cancer cells are particularly dependent on a process called homologous recombination to repair DNA and stay alive.
Now researchers at Washington University School of Medicine in St. Louis have found that a protein known as MDC1 has a role in homologous recombination. This discovery could be exploited in a two-pronged treatment strategy to eliminate cancer cells’ ability to repair DNA.
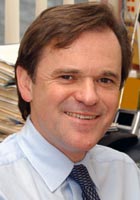
“Frequently cancer cells are more efficient at DNA repair than normal cells,” says Simon Powell, M.D., Ph.D., head of the Department of Radiation Oncology and a researcher with the Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital. “That’s what makes them resistant to drugs or radiation treatments that physicians use in an effort to damage cancer cells’ DNA and destroy them.”
But in light of their findings, Powell and his colleagues believe MDC1 — along with other proteins involved this repair pathway — may be good targets for dual-drug chemotherapeutic approaches that can completely knock out tumor cells’ ability to cope with DNA damage. Their study appears in the October issue of Nature Structural & Molecular Biology.
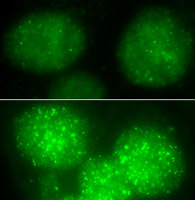
The research group discovered that MDC1, a protein previously recognized only for its function in sensing DNA damage and signaling its presence, also transports DNA-repair proteins to the site of DNA strand breaks. Without MDC1 to pave the way, repair happens slowly because the fix-it proteins have a hard time reaching damaged areas, which are buried in the tightly packed chromosomal material of the cell’s nucleus.
“MDC1 can bind to chromatin, the complex mixture of DNA and proteins that holds the genetic material,” Powell says. “Because of chromatin’s properties, getting into it to reach the DNA strand requires the right ‘passwords.’ MDC1 provides the DNA-repair proteins with this privileged access, and efficiently transports them to the site of damage so they can do their jobs.”
Chemotherapeutic strategies that reduce the activity of MDC1 could inhibit the ability of cancer cells to restore broken DNA. An accumulation of DNA damage would signal cells to initiate suicide pathways and die.
Although cells can find other ways to repair DNA, Powell says a dual strategy that used a second drug to knock out the survival mechanism in cells would deliver a one-two punch to tumors. It would force tumor cells to rely more heavily on homologous recombination repair and then block that route as well.
The research group already has begun studies that investigate the potential of targeting homologous recombination as a tumor-specific strategy. In this case, they are focusing on tumors with BRCA1 and BRCA2 deficiencies.
BRCA1 and BRCA2 are tumor suppressor proteins, and mutations in the genes for these proteins are widely known for being associated with a high risk of breast cancer in 5 to 10 percent of women. Tumors with BRCA1 and BRCA2 deficiencies have ineffective homologous recombination repair mechanisms, and Powell’s group has begun using this handicap to attack the tumors.
“BRCA1- and 2-deficient tumor cells represent a special case in which the homologous recombination repair pathway is already messed up,” Powell says. “So, we are trying to further sensitize BRCA1- and 2-deficient cancer cells to see if that approach can destroy them.”
Having uncovered a role for MDC1 in homologous recombination repair, the group now will be able to build on their BRCA1/BRCA2 research as they develop chemotherapeutic strategies that take advantage of MDC1’s cellular function.
Zhang J, Ma Z, Treszezamsk A, Powell SN. MDC1 interacts with Rad51 and facilitates homologous recombination. Nature Structural & Molecular Biology 2005 Oct;12(10):902-9.
Funding from National Cancer Institute supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Siteman Cancer Center is the only NCI-designated Comprehensive Cancer Center within a 200-mile radius of St. Louis. Siteman Cancer Center is composed of the combined cancer research and treatment programs of Barnes-Jewish Hospital and Washington University School of Medicine.