In laboratory tests, one very low dose of a drug was enough to show an effect on notoriously tenacious artery-clogging plaques. What kind of drug is that potent?
It’s not so much the drug itself as how it was delivered. Fumagillin — a drug that can inhibit the growth of new blood vessels that feed atherosclerotic plaques — was sent directly to the base of plaques by microscopically small spheres called nanoparticles developed by researchers at Washington University School of Medicine in St. Louis.
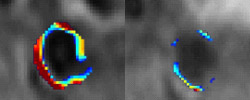
“Previously we reported that we can visualize plaques using our nanoparticle technology, but this is the first time we’ve demonstrated that the nanoparticles can also deliver a drug to a disease site in a living organism,” says Patrick Winter, Ph.D., research assistant professor of medicine. “After a single dose in laboratory rabbits, fumagillin nanoparticles markedly reduced the growth of new blood vessels that feed plaques.”
The researchers report their findings in the September issue of the journal Arteriosclerosis, Thrombosis, and Vascular Biology, and the article is now available on line.
An atherosclerosis plaque results when a buildup of cholesterol, inflammatory cells and fibrous tissue forms inside an artery. If a plaque ruptures, it can block blood flow to the heart or brain, causing heart attack or stroke.
While growing, plaques require an influx of nutrients, fats and cells, so they develop their own blood supply — minute blood vessels that grow within the wall of arteries and penetrate the plaque. Many believe that cutting off this blood supply could stabilize or reduce plaques. In previous studies, fumagillin has been shown to be an effective agent for stopping the process that creates new blood vessels.
Riding on the nanoparticles, fumagillin is carried to the site of new blood vessel formation and stays there thanks to a fellow nanoparticle passenger — a component that fastens the nanoparticles to cells found in newly developing blood vessels. Stuck in this position, the nanoparticle drops its load of fumagillin, concentrating it at the site of the atherosclerotic plaque.
In this study, the single dosage of fumagillin each rabbit received was 50,000 times lower than the total fumagillin dose used in an earlier experiment by another research group and yet reduced the growth of new blood vessels in plaques by 60 to 80 percent.
“Fumagillin can have neurocognitive side effects, causing injury to the brain at high doses,” Winter says. “The ability of the nanoparticles to concentrate the drug at the disease site allows the dose to be lowered. This could open the door for a lot of drugs that have failed to be approved because they caused too many side effects at a higher dose. It might pay to look at these drugs again and ask if placing them on these nanoparticles can help them be effective at a lower dose and clinically useful.”
The nanoparticles are the invention of Samuel Wickline, M.D., professor of medicine, of biomedical engineering, of physics and of cell biology and physiology, and Gregory Lanza, M.D., Ph.D., associate professor of medicine and biomedical engineering. Both are heart specialists at Barnes-Jewish Hospital.
The microscopic spheres are capable of carrying a variety of components at the same time and can be detected with standard MRI scans, making them useful for imaging disease sites while simultaneously treating them. Using the nanoparticles, a physician can confirm a drug has reached the desired location, measure the amount of drug at the site, and later check to see if the drug has affected the disease.
In the current study, the researchers fed rabbits a high-cholesterol diet for 80 days before treatment with fumagillin nanoparticles. The diet caused numerous small plaques in the rabbits’ aortas, but the plaques were considered to be at an early stage of growth. By demonstrating the utility of the nanoparticles for early intervention of atherosclerosis, the research group hopes that they can help alleviate the need for more invasive treatment of later-stage atherosclerosis.
“We wanted to go after the early stages of the disease when patients don’t yet need immediate intervention to prevent serious cardiac problems,” Winter says. “We think fumagillin nanoparticles potentially could be incorporated into a protocol that includes lipid-lowering statin drugs or dietary changes.”
Next, the research group plans to study the effect of fumagillin nanoparticles in the treatment of cancerous tumors. According to Winter, the use of inhibitors of blood vessel growth is a well-accepted therapy for cancer, suggesting the nanotechnology may prove beneficial in cancer therapy.
Winter PM, Neubauer AM, Caruthers SD, Harris TD, Robertson JD, Williams TA, Schmieder AH, Hu G, Allen JS, Lacy EK, Wickline SA, Lanza GM. Endothelial ανβ3 integrin-targeted fumagillin nanoparticles inhibit angiogenesis in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology September 2006, available on line ahead of print.
Funding from the National Institutes of Health, the American Heart Association and Philips Medical Systems supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.