See one, do one, teach one. That’s the philosophy under which Mary Klingensmith, M.D., and countless other surgeons trained. The adage refers to the medical tradition of doctors learning a surgical technique by observing it once before being expected to perform it independently the next time and then teach it to another surgeon in training.
But learning on the job is not the best way to teach surgical residents, says Klingensmith, who since 2001 has directed the surgical residency training program at the School of Medicine and Barnes-Jewish Hospital. It leaves patients vulnerable to inexperienced surgeons and doesn’t prepare young surgeons for the myriad complications that can arise in the operating room.
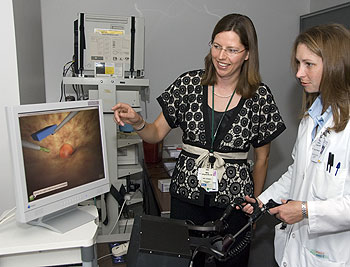
Klingensmith, associate professor of surgery, has been a driving force behind changing the way surgical residents are trained. She has spearheaded the development of a new curriculum that teaches residents surgical skills outside the operating room. Her efforts now ensure that the residents get lots of practice using teaching tools that range from low-tech plastic body parts to highly realistic computer simulations before residents ever put scalpel to flesh.
“It really makes intuitive sense,” says Klingensmith, “and we think it is making a huge difference. Patients are better off, and residents feel much more confident in their skills.”
Klingensmith knows firsthand the frustration of learning on the job. She has vivid memories of the first time she sutured a patient’s incision as a resident. “The attending surgeon was impatient with me, and the sutures didn’t look good,” she says. “I just remember the incredible pressure I felt knowing that this woman was going to live with my inadequacy.
“I had never had an opportunity to practice suturing before; no one had ever taught me in a relaxed environment, where I could really absorb it, think about it and practice it. And so I knew when I was in charge, I really wanted people learning from me to have that opportunity. It’s better for the patient, it’s better for the learners, it’s better for everybody.”
As a highly regarded young surgeon herself — she was chief surgical resident at Boston’s Brigham and Women’s Hospital and Harvard Medical School — Klingensmith has a keen understanding of the broad skills surgeons need to be successful. Her vision for residents’ education extends beyond their technical proficiency. She is a proponent of integrating medical ethics into surgeons’ training and is working at a national level to develop a standardized curriculum for surgical residents. In addition to skills training, the curriculum incorporates instruction for surgeons about how to interact with anesthesiologists, nurses, medical students and other members of the health-care team.
At the School of Medicine, Klingensmith also is director of the Surgical Skills Laboratory, where third-year medical students get their first exposure to basic skills such as suturing and tying knots, using a surgical stapler and learning how to hold a laparoscope — a long-handled instrument with a miniature camera attached — during surgery. First-year surgical residents also get a refresher course that covers all they need to know before setting foot into the operating room. “It’s all hands-on, out of the O.R. and low stress, so the students and residents can really learn,” she says.
In collaboration with David Murray, M.D., professor of anesthesiology, Klingensmith plays a key role in the Clinical Simulation Center. In 2005, she was named as one of the inaugural recipients of the Loeb Teaching Fellowships and used the funding to design a simulation curriculum for medical students and residents that focuses on task training — how to perform bedside, diagnostic and surgical procedures in a low-stress environment before making the transition to “real” patients.

The center also uses life-size mannequins to help simulate realistic scenarios a learner is likely to encounter in a clinical setting. “All the students and residents think the center is great, and it is an expected part of their education now,” Klingensmith says.
Her accomplishments have not gone unnoticed. “She has been just simply spectacular,” says Timothy Eberlein, M.D., the Bixby Professor and chairman of the Department of Surgery. “She’s a creative thinker and problem solver, and she’s held the department’s feet to the fire in our mission to make the surgical training program the best in the country. Mary has solidified this institution’s vision of what educating residents is all about.”
This academic year, Klingensmith will oversee 68 surgical residents and is responsible for ensuring that they meet all the requirements for board eligibility in surgery and accreditation by other professional organizations. If a resident has a problem — or the medical staff or a patient has a problem with a resident — Klingensmith is the go-to person. “I’m part mentor, part den mother, part disciplinarian, but it is all incredibly rewarding,” she says.
Klingensmith and her husband, Bruce Hall, M.D., Ph.D., associate professor of surgery, came to the School of Medicine from Harvard Medical School in 2000. Both were heavily recruited by Eberlein, who had been their faculty adviser when he was on the Harvard faculty. Hall is a cancer and endocrine surgeon who also teaches at the John M. Olin Business School. “Mary was a fabulous mentor and educator, even as a resident,” Eberlein says. “She would routinely take younger residents under her wing and teach and mentor them.”
|
Mary Klingensmith, M.D.
Family: husband Bruce Hall, M.D., Ph.D.; son, Tucker, 5; and daughter, Tenley, 3 Hometown: Beckley, W. Va. Education: B.A., Wellesley College, 1988; M.D., Duke University School of Medicine, 1992 Awards: Washington University Loeb Teaching Fellow; Outstanding Teacher Award, Association for Surgical Education; Finalist, Accreditation Council of Graduate Medical Education Parker J. Palmer “Courage to Teach” Award Outside interests: reading (especially Southern fiction), swimming, running, biking
|
The youngest of five children, Klingensmith was the only one to follow in her father’s footsteps. He was one of two general surgeons in a small West Virginia mining town. Although he graduated from Harvard Medical School and completed a surgical residency at Massachusetts General Hospital, he chose to open a surgical practice close to his hometown. “People would come up to me after church, telling me how great my daddy was, how he had saved their lives,” she says. “That was amazingly inspiring.”
During her residency in Boston, Klingensmith served on several education-related committees and realized she liked tackling governance issues. “It was then that I started to think about being involved in a systematic way in education and change in residency programs,” she says. “I knew that one of the things that I wanted to do was start a skills curriculum for residents where, for example, before you remove your first gall bladder in a patient, you have accomplished the procedure in a simulated environment.”
Like her father, Klingensmith is a general surgeon. She cares for underserved patients at the John Cochran Division of the St. Louis VA Medical Center and through Saint Louis ConnectCare, which provides health care to low-income patients who lack health insurance. She is grateful to provide care through this safety net and stresses to the residents what it means to treat these patients, many of whom have very different needs than those with health insurance.
As a doctor on the front lines of training residents, Klingensmith noticed that many lacked training in medical ethics. Klingensmith and Ira Kodner, M.D., the Solon and Bettie Gershman Professor of Surgery and director of the Center for the Study of Ethics and Human Values, now offer monthly pizza rounds, where residents can discuss current ethical problems. They also developed a curriculum for teaching ethics to surgical residents.
“Mary is becoming the preeminent teacher of medical ethics for surgical residents in the country,” says Kodner. “She knows better than anyone the ethical challenges the residents encounter, and her efforts to teach ethics are most important, on top of all her other responsibilities. And she’s an excellent clinical surgeon. You maintain no credibility in surgery if you’re not first and foremost a good surgeon.”
When Klingensmith is not keeping close watch over the surgical residents, she’s looking after her two young children, Tucker, 5, and Tenley, 3. The family can often be found at Soulard Market on Saturday mornings or at the Saint Louis Zoo or elsewhere in Forest Park on summer evenings. “We pick an animal of the week, read and talk about it, then have an end-of-the-week treat of a trip to the Zoo to see the animals in person,” Klingensmith says.