Researchers at Washington University School of Medicine in St. Louis have identified a new set of genetic markers for Alzheimer’s that points to a second pathway through which the disease develops.
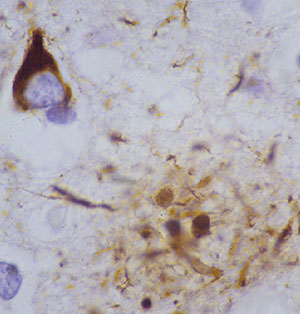
Much of the genetic research on Alzheimer’s centers on amyloid-beta, a key component of brain plaques that build up in the brains of people with the disease.
In the new study, the scientists identified several genes linked to the tau protein, which is found in the tangles that develop in the brain as Alzheimer’s progresses and patients develop dementia. The findings may help provide targets for a different class of drugs that could be used for treatment.
The researchers reported their findings online April 4 in the journal Neuron.
“We measured the tau protein in the cerebrospinal fluid and identified several genes that are related to high levels of tau and also affect risk for Alzheimer’s disease,” said senior investigator Alison M. Goate, DPhil, the Samuel and Mae S. Ludwig Professor of Genetics in Psychiatry. “As far as we’re aware, three of these genes have no effect on amyloid-beta, suggesting that they are operating through a completely different pathway.”
A fourth gene in the mix, APOE, had been identified long ago as a risk factor for Alzheimer’s. It has been linked to amyloid-beta, but in the new study, APOE appears to be connected to elevated levels of tau. Finding that APOE is influencing more than one pathway could help explain why the gene has such a big effect on Alzheimer’s disease risk, the researchers said.

“It appears APOE influences risk in more than one way,” said Goate, also a professor of genetics and co-director of the Hope Center for Neurological Disorders. “Some of the effects are mediated through amyloid-beta and others by tau. That suggests there are at least two ways in which the gene can influence our risk for Alzheimer’s disease.”
The new research by Goate and her colleagues is the largest genome-wide association study (GWAS) yet on tau in cerebrospinal fluid. The scientists analyzed points along the genomes of 1,269 individuals who had undergone spinal taps as part of ongoing Alzheimer’s research.
Whereas amyloid is known to collect in the brain and affect brain cells from the outside, the tau protein usually is stored inside cells. So tau usually moves into the spinal fluid when cells are damaged or die. Elevated tau has been linked to several forms of non-Alzheimer’s dementia, and first author Carlos Cruchaga, PhD, said that although amyloid plaques are a key feature of Alzheimer’s disease, it’s possible that excess tau has more to do with the dementia than plaques.

“We know there are some individuals with high levels of amyloid-beta who don’t develop Alzheimer’s disease,” said Cruchaga, an assistant professor of psychiatry. “We don’t know why that is, but perhaps it could be related to the fact that they don’t have elevated tau levels.”
In addition to APOE, the researchers found that a gene called GLIS3, and the genes TREM2 and TREML2 also affect both tau levels and Alzheimer’s risk.
Goate said she suspects changes in tau may be good predictors of advancing disease. As tau levels rise, she said people may be more likely to develop dementia. If drugs could be developed to target tau, they may prevent much of the neurodegeneration that characterizes Alzheimer’s disease and, in that way, help prevent or delay dementia.
The new research also suggests it may one day be possible to reduce Alzheimer’s risk by targeting both pathways.
“Since two mechanisms apparently exist, identifying potential drug targets along these pathways could be very useful,” she said. “If drugs that influence tau could be added to those that affect amyloid, we could potentially reduce risk through two different pathways.”
Funding for this research comes from the National
Institute on Neurological Diseases and Stroke (NINDS) and the National
Institute on Aging (NIA) of the National Institutes of Health (NIH).
Other funding was provided by AstraZeneca and the Barnes-Jewish Hospital
Foundation. For a complete list of groups that funded portions of this
study, please consult the “Acknowledgements” section of the paper. NIH
grant numbers: P30 NS069329-01, R01 AG035083, R01 AG16208, P50
AG05681, P01 AG03991, P01 AG026276, AG05136, P01 AG05131, R01 AG17917,
R01 AG15819, K08 AG034290, U01 AG024904, P30 AG010129 and K01 AG030514.
Cruchaga C, et al. GWAS of cerebrospinal fluid tau levels identifies novel risk variants for Alzheimer’s disease. Neuron, vol. 77(8), April 24, 2013 (published online April 4, 2013).
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.