In the hectic, tightly scheduled day at a memory clinic, doctors set aside blocks of time to meet with new patients suspected of having dementia. But much of that time is taken up gathering information needed to make a diagnosis, leaving little time for doctors to discuss the condition’s life-changing implications with patients and their families.
With the aim of streamlining the diagnosis of Alzheimer’s disease, a student-led team has designed an online app to help doctors more quickly evaluate patients. The app is being tested at Washington University School of Medicine in St. Louis.
“This app is not meant to replace the visit with the physician,” said MD/PhD student Robert Chen, who co-leads the student group known as Memento that designed the app. “It is meant to help physicians have more information about the patient before they are evaluated in person. With additional reliable and clinically relevant information in the hands of physicians beforehand, the hope is that physicians can make a diagnosis more quickly and confidently, and spend the extra time building a treatment plan and answering questions from patients and caregivers in the face of a devastating diagnosis.”
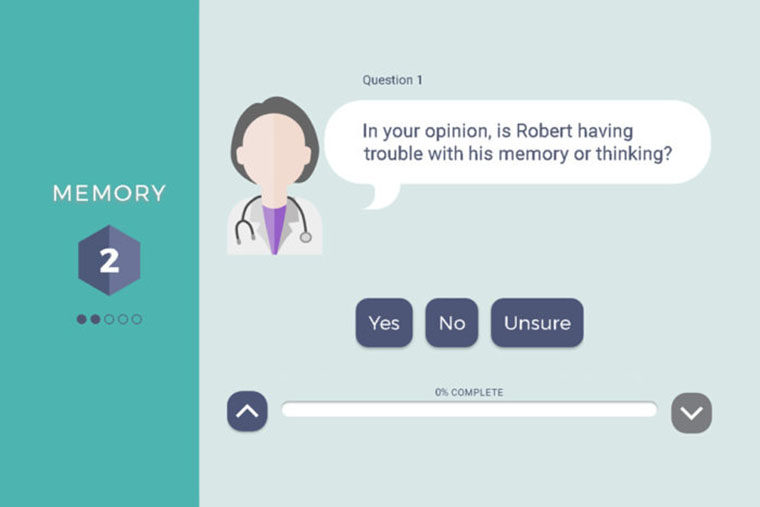
The app represents a collaboration between students at the Schools of Medicine, Arts & Sciences, and Engineering & Applied Science. It consists of 60 to 100 questions for a patient’s caregiver to answer on an iPad before the patient sees a dementia specialist. Once the questionnaire is complete, the app will generate a report with the information handily organized into categories that fit with the Clinical Dementia Rating Scale (CDR).
Developed at the School of Medicine, the CDR is the most commonly used tool for diagnosing dementia. It breaks down the patient’s symptoms into six domains – memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care – and provides a score for each.
“Having all the intake information from the patient and family summarized in alignment with the CDR could be really helpful,” said Nupur Ghoshal, MD, PhD, an assistant professor of neurology and of psychiatry, and the faculty mentor on the project. “It wouldn’t make the diagnosis for us, but it could feed into the thought processes that we go through as we evaluate each patient.”
The students have launched a six-month trial of the new app at the School of Medicine’s Memory Diagnostic Center. The caregiver of each new patient arriving for a dementia evaluation will be asked to use the app and answer the questions in the waiting room. Then, a doctor will examine the patient and make a diagnosis as usual.
Without seeing the patient, another doctor in the clinic will review the app’s report and make a diagnosis as well. With feedback from the physicians, the students will apply machine-learning techniques to identify which questions provided helpful information that led to an accurate diagnosis.
“We will determine which questions were most indicative, which were the least indicative and, at any given point, what’s the next best question to ask,” said Allen Osgood, who co-leads the Memento team and earned bachelor’s and master’s degrees in computer science from the School of Engineering & Applied Science in May.
The doctors also will note how long it takes them to read and digest the report, so the students can estimate how much time the app saves.
Building the app required not just an understanding of how Alzheimer’s disease is diagnosed and treated, but programming and design, as well.
“One of the students, Jenny Liu, really helped make the app appealing and intuitive,” Ghoshal said. “It doesn’t look like your standard questionnaire. We hope that a warmer design will help caregivers feel more comfortable answering these questions.”
The student group was brought together by Sling Health Network, a student-run biotechnology incubator that provides resources, training and mentorship to teams of students tackling clinical problems by developing innovative solutions. Along with Chen and Osgood, the team includes: Jenny Liu, who earned a bachelor’s degree in biology in 2016; Morgan Redding, who earned a bachelor’s degree in computer science with a second major in mathematics in May; and Stolovitz, who earned a bachelor’s degree in computer science with minors in design and physics, also in May.
If the trial is successful, the team plans to work with the Alzheimer’s Association to launch the app at other St. Louis-area neurology clinics in the future. Last summer, the team won $10,000 as a finalist for the Student Technology Prize for Primary Healthcare from the Gelfand Family Charitable Trust.
“Having the chance to build things from the ground up in an environment where there is no clear answer is definitely a testament to the education we’ve received at Washington University,” Osgood said. “Having the ability to go in and work with professionals to learn HIPAA compliance and systems security and all the different things we need to implement this on the user and technical side has been instrumental to the success of the project.”
Comments and respectful dialogue are encouraged, but content will be moderated. Please, no personal attacks, obscenity or profanity, selling of commercial products, or endorsements of political candidates or positions. We reserve the right to remove any inappropriate comments. We also cannot address individual medical concerns or provide medical advice in this forum.