Studying mice, scientists have shown that boosting the activity of specific immune cells in the heart after a heart attack can protect against developing heart failure, an invariably fatal condition. Patients with heart failure tire easily and become breathless from everyday activities because the heart muscle has lost the ability to pump enough blood to the body.
The study, by researchers at Washington University School of Medicine in St. Louis, could lead to new therapies that reduce the risk of developing heart failure after a heart attack, severe viral illness or other cardiac injury. Damage to the heart muscle often causes progressive inflammation, a major driver of heart failure. According to the Centers for Disease Control and Prevention, about 5.7 million American adults have heart failure.
The research is published Nov. 1 in the journal JCI Insight.
“Heart failure remains a major problem, with half of all patients dying within five years of diagnosis,” said senior author and cardiologist Abhinav Diwan, MD, associate professor of medicine. “There are therapies that can relieve symptoms and extend life, but we need to do better. Our research is focused on finding ways to boost the immune system to help the heart heal after injury, which can prevent heart failure from progressing.”
During a heart attack, blood supply to a portion of the heart muscle is cut off, starving the heart muscle of oxygen and leading to the death of cardiac tissue. If the patient survives, the body’s immune cells respond to the heart injury to get rid of dead tissue and begin the healing process.
“These specific immune cells — macrophages — eat up the dead cells damaged during the heart attack and stimulate the heart to repair itself, but if the macrophages stick around too long, they become inflammatory and drive the damage that leads to heart failure,” Diwan said.
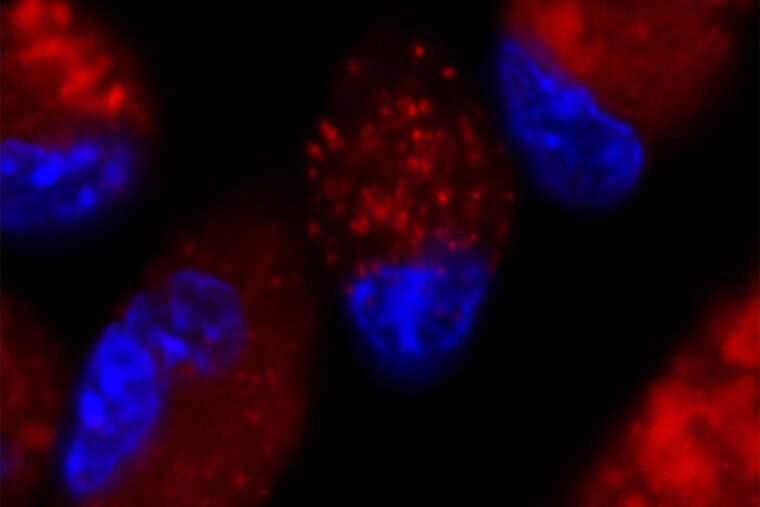
In the new study, the researchers, including first author Ali Javaheri, MD, PhD, an instructor in medicine in the Cardiovascular Division, have found a way to supercharge these macrophages, increasing their abilities to digest and dispose of damaged heart tissue left in the wake of a heart attack. The key is in stimulating specialized sacs called lysosomes, which are inside immune cells. Digestion and waste disposal take place inside lysosomes.
The researchers activated a molecule — called TFEB — that spurred heart macrophages to make more lysosomes. In particular, TFEB also helped lysosomes digest lipids, or fat molecules, more effectively.
“Macrophages are the ‘eating cells,’ and lysosomes are like their stomachs,” Diwan said. “When we boosted the number of lysosomes, we enhanced their ability to digest damaged heart cells. Instead of provoking heart failure, this lowered inflammation and helped reduce the development of heart failure in the mice.”
The researchers are planning to investigate various small molecules as potential drug therapies that could activate TFEB and stimulate these important immune cells to improve their capacity to heal the heart following a cardiac injury, whether due to heart attack, viral infection or other forms of heart damage.
Comments and respectful dialogue are encouraged, but content will be moderated. Please, no personal attacks, obscenity or profanity, selling of commercial products, or endorsements of political candidates or positions. We reserve the right to remove any inappropriate comments. We also cannot address individual medical concerns or provide medical advice in this forum.