Researchers at Washington University School of Medicine in St. Louis appear to have discovered a way to make radiation therapy for colorectal cancer more effective by inhibiting a protein found in cancer cells in the gut. The approach also helps protect healthy tissue from the negative effects of radiation.
Studying cells, mice and tumor samples from patients with cancer, the scientists targeted an enzyme known as indoleamine 2,3 dioxygenase 1 (IDO1). Treating tumor cells with a drug that inhibits that enzyme didn’t eliminate colorectal cancer completely. Nor did radiation therapy alone. But when the researchers combined the drug with radiation, cancer cells grew more slowly and, in some cases, stopped multiplying altogether.
The findings are published online March 3 in the journal Cancer Immunology Research.
Radiation therapy is a mainstay of colorectal cancer treatment. Depending on the radiation dose, the therapy can have side effects, such as fatigue, skin issues, and bowel and bladder problems. But the therapy also can slow tumor growth or even destroy tumor cells.
“In every model we studied, the combination therapy showed great promise,” said senior author Matthew A. Ciorba, MD, associate professor of medicine and director of the Inflammatory Bowel Disease Center at Washington University. “Neither strategy was wholly effective by itself, but the combination was very effective, leading to more cell death within tumors, higher activation of the immune system and better protection of healthy tissue.”
Excluding certain skin cancers, colorectal cancer is the third-most common type of cancer in the United States and the second-leading cause of cancer death. About 145,000 new cases were diagnosed in 2019, with an estimated 51,000 deaths. Death rates from colorectal cancer have been dropping, probably because screening can detect polyps before they become cancerous, and doctors can remove such polyps before they become a problem. But when cancer is more advanced at detection, effective treatments remain elusive.
Ciorba, a gastroenterologist, had been studying the IDO1 protein in research aimed at treating inflammatory bowel diseases such as Crohn’s disease and colitis. The IDO1 gene is very active in those disorders, as it is in colorectal cancer.
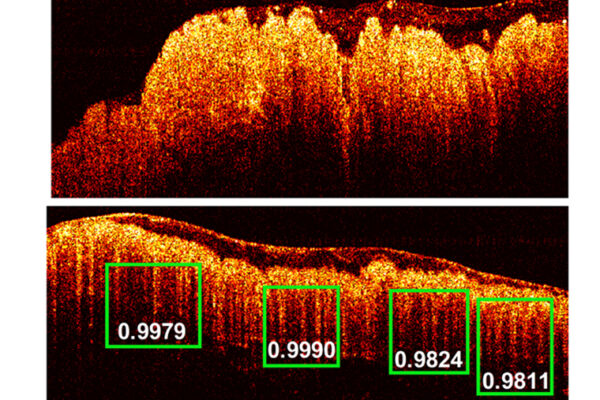
In this study, the researchers treated colon cancer cell lines with radiation and found that the cells made more IDO1 protein after a single dose. They also looked at tumor samples from patients with colorectal cancer and found that radiation caused those cells to make more of the protein. Further experiments suggested the protein might be protecting cancer cells from the effects of radiation.
“In earlier studies, we had found that the absence of the protein made mice less likely to develop colorectal cancer when the animals were exposed to carcinogens,” said the paper’s first author, Baosheng Chen, a research instructor in medicine in the gastroenterology division. “However, blocking the protein using the inhibitor was not as effective as expected in animal models of colorectal cancer. So the focus of our investigation was to see whether we could combine this drug inhibitor with another agent we already use, such as radiation, to treat cancer more effectively.”
Using techniques to block the IDO1 gene, as well as the drug epacadostat to block the protein’s activity, made radiation more effective in slowing tumor growth. Combining the strategies contributed to tumor shrinkage in 40% of the tumors the researchers studied. In mice, combining radiation with inhibition of the protein also resulted in tumors located away from the primary cancer shrinking or growing more slowly. And in other experiments, the combination therapy prevented recurrence of the cancers.
“It acted almost like a vaccine,” Ciorba said. “Mice that received the combined therapies were less likely to develop other cancers of the same type.”
The researchers now are testing the approach in people with colorectal cancer.
“Our patients with rectal cancers receive radiation first, and then they have chemotherapy,” said study investigator Haeseong Park, MD, assistant professor of medicine and a medical oncologist. “After radiation and chemotherapy, patients are re-evaluated, and if they still have evidence of cancer, they get surgery. Currently, more than half of our patients eventually need surgery, but our ongoing clinical trial is designed to combine radiation with inhibition of IDO1 to lower the percentage of patients who eventually need surgery, while also protecting them from radiation’s toxicities.”
Because the protein also is overexpressed in other abdominal and pelvic cancers, Ciorba explained that blocking its activity may be helpful in other types of cancer, too.
“It may be possible to expand this strategy and use it in treating esophageal, cervical and ovarian cancer,” he said.


Comments and respectful dialogue are encouraged, but content will be moderated. Please, no personal attacks, obscenity or profanity, selling of commercial products, or endorsements of political candidates or positions. We reserve the right to remove any inappropriate comments. We also cannot address individual medical concerns or provide medical advice in this forum.