Tip sheets highlight timely news and events at Washington University in St. Louis. For more information on any of the stories below or for assistance in arranging interviews, please see the contact information listed with each story.
Finding SARS sooner
Washington University researchers develop a test to quickly diagnose SARS
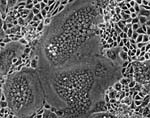
Rapid and accurate diagnosis is critical for providing optimum care for patients with SARS and for helping contain the disease and protecting the community. If someone with a severe respiratory illness comes to Barnes-Jewish Hospital or St. Louis Children’s Hospital, emergency department physicians now should be able to tell whether the disease is SARS within a few hours. A team of researchers, led by Michael J. Holtzman, M.D., the Selma and Herman Seldin Professor of Medicine and professor of cell biology and physiology at Washington University School of Medicine in St. Louis, developed a diagnostic tool that allows for quick identification of whether a person with respiratory disease has SARS. They also can determine the severity of the infection, and the test can detect the SARS virus even if very few virus molecules make it into the test sample.
Pin prick
New technique makes IV starts less painful

Neuroscience researchers at Washington University School of Medicine in St. Louis are studying the brains of patients with Tourette Syndrome (TS) to see whether they can use sophisticated imaging techniques to identify differences in the dopamine system of people with the tics that characterize TS. A team of researchers, led by Kevin J. Black, M.D., assistant professor of psychiatry, neurology and radiology at Washington University School of Medicine, is using PET imaging to see what the brain does in response to levodopa, a natural amino acid that has been used for many years to treat movement disorders, such as Parkinson’s disease. With PET imaging, the researchers can measure the boost in the brain’s dopamine levels in response to the drug both in people with Tourette Syndrome and in those who do not have tics. By identifying differences, they hope to isolate the causes of tics and to help people with TS control or eliminate them.
Is there a hospitalist in the house?
A new breed of specialists cuts lengths of hospital stays and lessens demands on primary care doctors

In today’s era of managed care, most physicians have fewer inpatients, and that makes it hard for many to justify spending time at the hospital with those patients. Mark S. Thoelke, M.D., clinical director of the hospitalist service at Barnes-Jewish Hospital and assistant professor of medicine at Washington University School of Medicine in St. Louis, says because hospitalist physicians do not maintain outpatient practices, they can spend all of their time in the hospital and are available to treat a wide range of patients. That also allows for improvements in outpatient care because with their inpatients cared for by hospitalists, primary care physicians can focus even more of their time on the needs of the outpatients who make up the vast majority of their practices.