Nearly half of all patients with amyotrophic lateral sclerosis (ALS), a fatal neuromuscular disorder, develop cognitive problems that affect memory and thinking. Why a disease that primarily affects movement also disrupts thinking has been unclear. But now, an international team of researchers has identified genetic links between ALS and frontotemporal dementia, a rare disorder marked by deterioration in behavior and personality, language disturbances and poor impulse control.
ALS initially damages neurons in the spinal cord while frontotemporal dementia mainly affects neurons in the brain. But the newly identified genetic connections between the two disorders may explain why they share some of the same features. Further, the links suggest that some drugs developed to treat ALS also may work against frontotemporal dementia and vice versa.
The new findings are published April 9 in the journal JAMA Neurology.
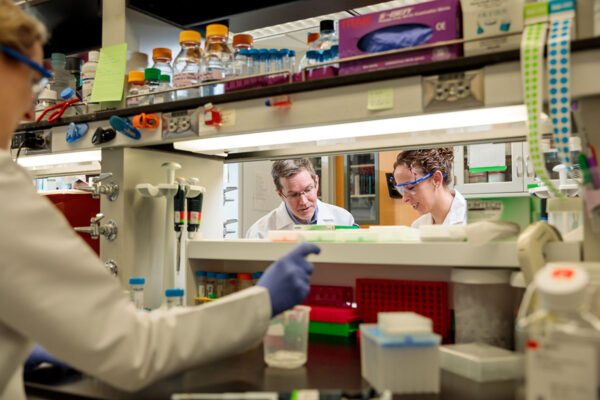
“Although there was clinical evidence that frontotemporal dementia and ALS may be connected, we didn’t fully understand the genetic connection,” said the study’s first author, Celeste M. Karch, assistant professor in the Department of Psychiatry at Washington University School of Medicine in St. Louis. “Identifying these genes connected to both disorders is important because, potentially, the shared genetic risk may point to common pathways that could be targeted therapeutically, raising the possibility that we might be able to treat the two devastating diseases with a single strategy.”
There are about 6,000 new cases of ALS diagnosed each year in the United States, and at any given time, there will be about 20,000 people in the country living with the disease. The total number of frontotemporal dementia patients in the U.S. is unclear, though it is estimated to account for about 20 percent of early-onset dementia cases.
Karch and co-author Rahul S. Desikan, MD, PhD, an assistant professor of neuroradiology at the University of California, San Francisco, led the analysis of data from several genetic studies. This included information from almost 125,000 individuals with various neurological disorders — such as ALS, frontotemporal dementia, Alzheimer’s disease and Parkinson’s disease — as well as from healthy control subjects of the same age ranges. Patients ranged in age from their 50s to 70s.
The analysis identified other common genetic variations that had not been linked to ALS. For example, common variants near the MAPT gene, which makes the tau protein, previously had been associated with diseases including frontotemporal dementia and Alzheimer’s disease. But the gene hadn’t been linked to ALS.
“This is one of the first genetic connections between ALS and MAPT,” Karch said. “Rare mutations and common variations in MAPT can increase risk for diseases that involve the tau protein, but now we’ve shown that some of the same, common gene variants also increase risk of ALS. We don’t think about the tau protein in ALS as we do with Alzheimer’s and other so-called tauopathies, but these findings raise the possibility that tau-mediated therapies may be useful in treating some ALS patients.”
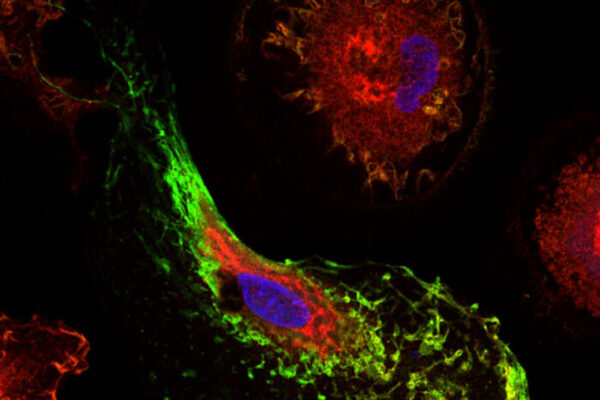
The researchers also identified variations in a second gene, BNIP1, which normally plays an important role in protecting against cell death. They found that variants in BNIP1 increased the risk of both ALS and frontotemporal dementia. They also found that levels of the protein made by that gene were altered in people who had ALS and in patients with frontotemporal dementia, suggesting the BNIP1 may be a potential therapeutic target for both disorders.
Karch and Desikan agreed that the study demonstrates it’s possible for scientists to combine existing data to identify new disease risk factors that wouldn’t be obvious in smaller studies.
“I think this kind of big-data approach can point us in the right direction on where to start for better understanding ALS, which remains poorly understood,” Desikan said.