By age 40, almost everyone’s arteries have begun to harden as deposits of fat and cholesterol build up on the inside of the blood vessels. Clumps big enough to obstruct blood flow can starve tissues of needed oxygen and nutrients. But even small deposits can be lethal, if they release fragments that clog downstream blood vessels. These unstable deposits – known as vulnerable plaque – can trigger heart attacks and strokes in seemingly healthy people.
Now, the National Heart, Lung and Blood Institute of the National Institutes of Health (NIH) has given Yongjian Liu, associate professor of radiology at Mallinckrodt Institute of Radiology (MIR) at Washington University School of Medicine in St. Louis, a $5.1 million Emerging Investigator Award to find a way to reduce the risk of sudden injury or death by identifying vulnerable plaque and treating it. The prestigious award – which will support Liu’s work for the next seven years – represents a vote of confidence in his ability to tackle a critical threat to human health.
“Plaque is the troublemaker behind the scenes,” Liu said. “What you see is a person having a heart attack or stroke, but backstage there is a vulnerable plaque that has broken off and clogged a blood vessel. The problem is that there’s no way to predict the rupture of a plaque. We can tell that someone has plaque, but not whether it increases the risk of a serious cardiovascular event like heart attack or stroke.”
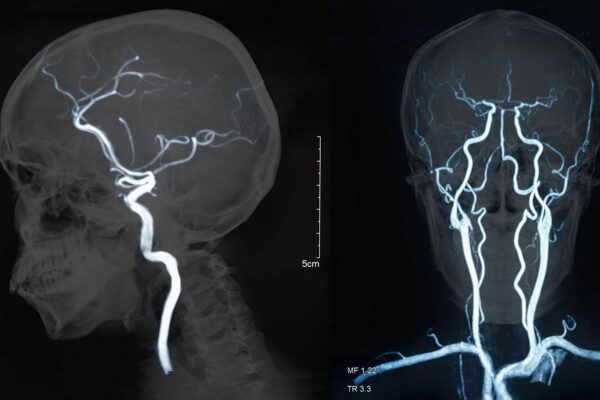
Cardiovascular disease is the leading cause of death in the U.S., and more than half of those deaths are linked to atherosclerosis, or hardening of the arteries due to plaque buildup. Exercise stress tests and X-ray and CT scans can detect large plaque deposits that narrow arteries and obstruct circulation. Physicians treat such obstructions either with surgery or medications to open a path for blood flow.
But for people with smaller plaque deposits, doctors struggle to decide whether and how to intervene. If the plaque lies in arteries in the neck, which supply blood to the brain, doctors often remove it to avert a potential stroke. But experts say that up to 98 percent of such surgeries could be avoided if we had a better way of distinguishing vulnerable plaque deposits from less-dangerous ones.
“There’s really no way to identify people at risk unless you do imaging,” Liu said. “Genotyping and blood chemistry don’t reveal what’s going on inside the blood vessels. Only imaging lets us look inside a person’s body and quantify the severity of disease.”
This grant provides support for Liu and colleagues including Robert J. Gropler, MD, the senior vice chair and division director of radiological sciences at MIR, to design PET-based, noninvasive imaging tools to distinguish vulnerable plaque from other kinds of plaque in the body. PET scans rely on tracers – specialized probes linked to radioactive compounds that can be detected by PET scanners – to identify signs of disease in the body. MIR, where Liu conducts research, is one of the few sites in the country with the equipment and expertise to shepherd a new PET tracer from the design stages through animal studies to clinical trials.
Plaque containing inflammatory cells and proteins are more likely to rupture, so Liu is designing probes to pick up signs of inflammation within plaque. Then, along with colleagues including Daniel Kreisel, MD, PhD, a professor of surgery, Liu will study mice with atherosclerosis and samples of blood vessels from people who underwent plaque-removal surgery to assess whether the tracers can reliably detect vulnerable plaque.
Identifying plaque at risk of breakup is step one on the path to preventing unexpected strokes and heart attacks. Step two is making such plaque less prone to shedding dangerous fragments into the bloodstream. Tamping down inflammation within plaque might make it less susceptible to disintegration and therefore less likely to cause a catastrophic blood clot, Liu said. With Craig J. Hawker, PhD, a professor of materials science at the University of California, Santa Barbara, Liu plans to load anti-inflammatory compounds onto nanoparticles and couple the loaded nanoparticles to probes specific for vulnerable plaque. In this way, he will be able to deliver anti-inflammatory drugs precisely where they are needed.
“The goal is really individualized, targeted treatment,” Liu said. “Right now, we don’t know who is at risk and even if we did, we can’t deliver drugs precisely and efficiently. With imaging, we’ll be able to identify vulnerable plaque, deliver treatment directly to it, and see whether the treatment is effective. In a few years, I hope to be able to deliver a toolbox that will allow doctors to find patients at risk and treat them before they have a heart attack or stroke.”