The battle against HIV increasingly looks winnable, and Washington University in St. Louis is helping lead the charge. Rupa Patel, MD, an assistant professor of medicine, has received a grant for $3.9 million from the Centers for Disease Control and Prevention (CDC) to establish a regional resource center at the university to aid HIV prevention efforts in 12 Midwestern states.
The center is part of a nationwide push to end the HIV epidemic in the U.S.
“There’s a medication, a pill you can take every day, that protects you from getting HIV,” Patel said. “With this new medication, we’ve seen rates of new infections reduced fairly quickly around the world. So the U.S. political and health sectors came together and said, ‘Let’s end HIV in the U.S.’ At the federal level, there is a goal of ending the HIV epidemic in the U.S. by 2030. Our contribution to that goal is that we’re going to make sure that this pill gets to everyone who would benefit from it in the Midwest.”
About 39,000 people become infected with HIV in the U.S. every year, usually through sexual contact or by sharing needles with someone with HIV to inject drugs. With treatment, people with HIV can live as long as people without HIV. The virus never goes away, but people with HIV who take their medicine regularly are unlikely to pass the virus to someone else. But not everyone infected with HIV receives therapy, and so the virus continues to spread.
The development in 2012 of preexposure prophylaxis, or PrEP, changed the game of HIV prevention. One PrEP pill a day cuts risk of sexual transmission by 92 percent and of blood-borne transmission by more than 70 percent. When combined with tried-and-true methods of HIV prevention such as condoms and needle exchanges, PrEP could be the tool that finally puts a stop to new HIV infections.
As part of the federal initiative to end the HIV epidemic, the CDC launched a five-year, $120 million program to strengthen the nation’s HIV-prevention efforts and tapped 17 organizations to implement the program.
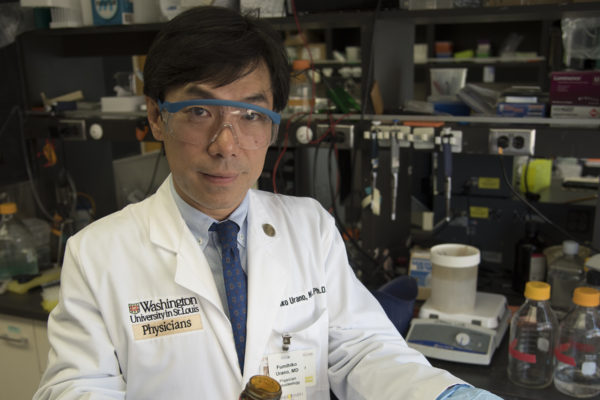
Patel and co-principal investigator Bradley Stoner, MD, PhD, an associate professor of anthropology in Art & Sciences and of medicine at the School of Medicine, were selected to establish the Midwest Capacity Building Assistance Network to provide individualized expertise, technology and resources to Midwestern organizations that want to scale up HIV prevention and PrEP services.
Both Patel and Stoner are experienced in the field. Patel directs Washington University’s PrEP Program, which provides PrEP care to HIV-negative people and which collaborated with the Missouri Department of Health to create a website and toolkit with resources for providers and consumers of PrEP care. Stoner is the medical director of the CDC-funded St. Louis STD/HIV Prevention Training Center, which provides health-care professionals with the latest research on sexually transmitted diseases. They will assist groups working in hard-hit communities in Missouri, Illinois, North Dakota, South Dakota, Nebraska, Kansas, Minnesota, Iowa, Wisconsin, Michigan, Indiana and Ohio.
“Every town, every region, has community-based organizations that do HIV prevention, but sometimes they run into problems they don’t know how to solve,” Stoner said. “Before you can give someone PrEP, you have to take a blood draw and make sure their kidney function is OK. Maybe they don’t know how to pay for that. Or they have people who are scared to get an HIV test, and the organization needs to know how to educate their community in a culturally sensitive way. We’re here to help them overcome these kinds of problems.”
Along with individualized advice and support, the center will provide workshops and training to share best practices for providing HIV testing and PrEP in the Midwest. Nancy Mueller, the assistant dean for planning and evaluation at the university’s Brown School, and colleagues at the Brown School Evaluation Center will help assess the center’s effectiveness at supporting HIV prevention efforts.
“HIV is an urban and a rural epidemic in the Midwest,” Patel said. “You can’t take the models verbatim from San Francisco or New York and try to apply them in Cleveland or Detroit. We have designed tools, standard operating procedures, checklists that are a lot friendlier to clinics that are smaller. The goal is not to say that every organization needs to start PrEP right now. But if we take the time to understand what their challenges are, we can help make sure that every organization gets their clients the best care they can. And in the long run, that will help put a stop to this epidemic.”