Alzheimer’s disease is the most common form of dementia, affecting more than 5 million people in the U.S., but doctors have limited advice on how to protect against it. The disease develops silently in the brain for two decades or more before people begin showing the characteristic signs of forgetfulness and confusion. Understanding that silent phase could be key to preventing this devastating condition.
Two studies from Washington University School of Medicine in St. Louis could help identify people at high risk of developing Alzheimer’s dementia and point to strategies for prevention. One study found that different forms of a key Alzheimer’s protein known as tau arise in a predictable sequence as the disease develops, starting more than 20 years before symptoms appear. The other showed that lack of sleep increases levels of a particular form of tau that is harmful. The studies are available online in Nature Medicine and Annals of Neurology.
The findings help explain why poor sleep is linked to increased risk of Alzheimer’s dementia and could lead to ways to identify where people stand on the road to Alzheimer’s.
“The goal is to halt the Alzheimer’s process before people develop symptoms,” said Randall J. Bateman, MD, the Charles F. and Joanne Knight Distinguished Professor of Neurology and the co-senior author of both studies. “To do that, we need a better understanding of how tau contributes to Alzheimer’s, so we can identify targets to develop new Alzheimer’s treatments.”
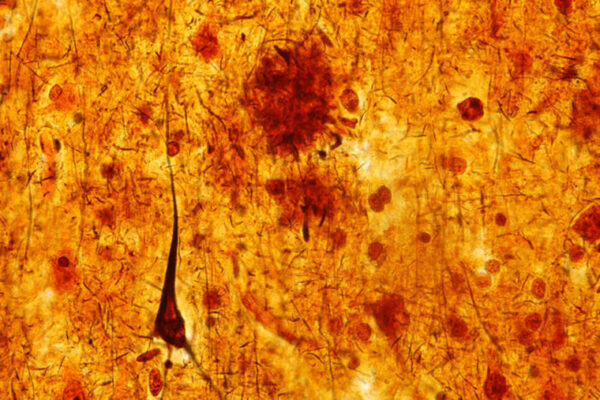
Alzheimer’s disease is linked to two main proteins: amyloid and tau. Both are normal brain proteins that become harmful when they collect into clumps. Amyloid plaques first appear two decades or more before cognitive symptoms arise. Tau tangles form later, just as damage becomes visible on brain scans and cognitive skills begin to decline.
Bateman, co-senior author Eric McDade, DO, and colleagues including first author Nicolas Barthélemy, an instructor in neurology, suspected that tau might start undergoing changes very early in the disease process that eventually results in the formation of tangles – and cognitive decline.
To find out, they studied people enrolled in the Dominantly Inherited Alzheimer Network (DIAN). Such participants have rare genetic mutations that cause them to develop Alzheimer’s at young ages, around the same ages their parents developed the disease. While devastating for families, these mutations allow researchers to know who will develop the disease and when.
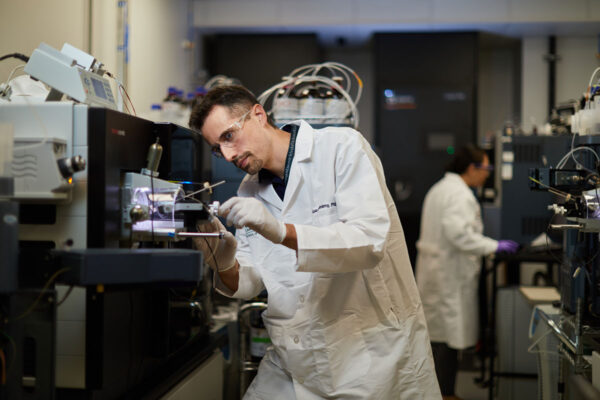
The researchers analyzed samples of cerebrospinal fluid — the fluid that surrounds the brain and spinal cord — from 370 DIAN participants. They were looking for tau that had been chemically modified by the addition of a phosphate group, a process known as phosphorylation. They detected phosphorylated forms of tau in some of the earliest samples – around the same time amyloid plaques appear and long before tau tangles arise.
“Although we can’t make causal claims from this study, we suspect that the development of plaques drives the tau changes,” McDade said.
Further, the forms of phosphorylated tau arose in a specific sequence. The researchers found that one form — phosphorylated tau-217 — arose 21 years before the expected age of symptom onset and stayed high until just before signs of cognitive decline became detectable. Other phosphorylated forms appeared later. Altogether, their data outlined a clear sequence of tau changes in the years leading up to Alzheimer’s dementia.
“By looking at tau phosphorylation, we can pinpoint where people are in the disease,” McDade said. “If everything is normal except for one of these, then you have a long way to go before you develop symptoms. But if a lot are abnormal, you’re within a few years of developing symptoms.”
Separately, Bateman, Barthélemy and co-senior author Brendan Lucey, MD, an assistant professor of neurology and director of the Washington University Sleep Medicine Center, investigated the effect of sleep on phosphorylated tau. Poor sleep, such as from sleep apnea, has been linked to risk of developing Alzheimer’s dementia.
The researchers studied eight people ages 30 to 60 with no sleep or cognitive problems. The participants were assigned randomly to one of three conditions: having a normal night’s sleep without any sleep aids; staying up all night; or sleeping after treatment with sodium oxybate, a prescription medication for sleep disorders.
The researchers took samples of the fluid that surrounds the brain and spinal cord every two hours over a 36-hour period to monitor how tau phosphorylation patterns change with time of day and different sleep conditions. All eight participants returned four to six months later to undertake a second condition, and four people completed all three.
After a sleepless night, phosphorylated tau-217 in the cerebrospinal fluid rose 60% to 80% over baseline levels. There was no such rise after a night of normal sleep or after sleeping with the aid of a drug.
“The changes to tau phosphorylation that we’re seeing in this study could explain how sleep deprivation promotes the development of Alzheimer’s disease,” Lucey said. “We’ve previously shown that sleep deprivation increases amyloid-beta in the fluid around the brain. If someone has a sleep disturbance for many years and they’re constantly having exposure to increased amyloid-beta and tau phosphorylation, that could promote the spread of destructive forms of tau and lead to brain damage and cognitive problems.”