Almost a year ago, COVID-19 began its global rampage, going on to infect about 69.5 million people and kill about 1.6 million as of early this month. From the beginning, most scientists have said that COVID-19 is deadlier than the seasonal flu, while fringe theories have circulated widely, suggesting it is less deadly or flu’s equal.
Evidence is accumulating, however, to show just how much deadlier COVID-19 is compared with the flu and the extent of complications related to the two illnesses.
The new research — a deep dive into federal data by researchers at Washington University School of Medicine in St. Louis and Veterans Affairs St. Louis Health Care System — reveals a clearer distinction between the two contagious viruses: Among hospitalized patients, COVID-19 was associated with an increased need for ventilators, more admissions into intensive care units (ICUs), longer hospital stays and nearly five times the risk of death than faced by those with the flu.
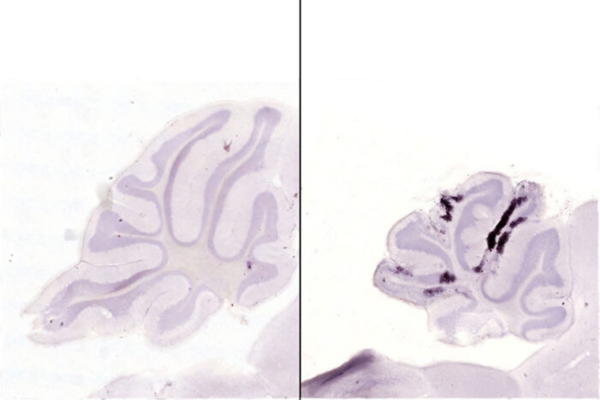
And although both illnesses attack the lungs, the analysis showed COVID-19 also can damage other organs. It revealed that COVID-19 was associated with a higher risk of complications such as acute kidney and liver damage, as well as heart disorders, stroke, severe septic shock, low blood pressure, excessive blood clotting and new-onset diabetes.
The findings are published online Dec. 15 ET in the journal The BMJ.
“Many high-profile, public comparisons between COVID-19 and the flu have been made; however, those comparisons mostly were drawn using disparate data and statistical methods that have resulted in a lot of conjecture,” said senior author Ziyad Al-Aly, MD, assistant professor of medicine at Washington University. “Our research represents an apples-to-apples comparison between the two diseases.”
The U.S. is experiencing its highest surge in COVID-19 cases — and at the same time flu season typically begins.
“Having a uniform comparison of data helps with disease prediction models, preparation and prevention efforts,” Al-Aly added. “The findings may inform the discussion in the U.S. and abroad about the comparative risks of COVID-19 and seasonal influenza, and may help the ongoing effort to manage the COVID-19 pandemic.”
For the study, the researchers analyzed de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated health-care delivery system. The researchers examined information involving 3,641 patients hospitalized in the U.S with COVID-19 at some point from Feb. 1 through June 17, as well as 12,676 patients hospitalized with the flu at some point from Jan. 1, 2017, through Dec. 31, 2019. The average age of patients with either COVID-19 or the flu was 69.
Among the 12,676 patients hospitalized with flu, 674 (5.3%) died, and of 3,641 patients hospitalized with COVID-19, 676 (18.5%) died. When the researchers adjusted for differences in age, race, clinical conditions and other factors, those infected with the novel coronavirus were nearly five times more likely to die than those with influenza.
In addition, on average, the COVID-19 patients were four times more likely to require breathing machines and almost 2.5 times more likely to be treated in the ICU. Also, COVID-19 patients were more likely to be hospitalized longer, an average of three extra days.
One of the biggest surprises in the study was the finding of a higher risk of developing diabetes among COVID-19 patients than flu patients — nine more cases per 100 people. “These patients didn’t have diabetes until they got COVID-19,” Al-Aly said. “Then their blood sugar spiked, and they needed huge doses of insulin. Is the diabetes reversible, or will it require long-term management? Will it be Type 1 or Type 2 diabetes? We just don’t know because COVID-19 barely existed a year ago.”
The data analysis also showed that the COVID-19 patients most at risk for death were those 75 years old and older who also had chronic kidney disease or dementia; and African Americans who were considered medically obese, or who had diabetes or kidney disease.
“A deeper understanding of the health risks of COVID-19 helps to anticipate demand for health-care services and to project mortality with greater accuracy,” Al-Aly added. “We know so little about COVID-19 because of its newness. I’m not sure why Black patients suffer and die more. My hunch is that the cause relates to racial disparities in health care, but there could be other factors that we don’t yet know.”
The researchers also found that, when compared with the flu, COVID-19 was associated with a higher risk of acute kidney damage and severe sepsis shock — both at six more cases on average per 100 hospitalized patients.
Compared with flu patients, people with COVID-19 also required more medications to treat severely low blood pressure, a condition that can lead to organ damage and death – 11.5 more people per 100 people.
“We can call COVID-19 a respiratory virus all we want, but if you look at the associated clinical consequences, it can cause significant damage to the brain, liver, heart, kidneys and blood-clotting systems,” Al-Aly said. “It’s a destructive virus.”
Al-Aly continued: “It’s quite possible that a year or five years from now there could be COVID-19 complications that we haven’t considered. Already, we’re aware of the long-haulers, or people who get COVID-19 but never fully recover. They might feel an ongoing malaise or extreme fatigue or experience appetite changes. Is it a lingering infection? Low-grade inflammation? An autoimmune disease? We are still learning. Even for people who are fortunate to survive the acute COVID-19 illness, they may be forever scarred by the lasting impact of its long-term clinical complications. The more we understand, the better we can benchmark health-care resources and treat patients.”