A study in mice — led by researchers at Washington University School of Medicine in St. Louis — shows that a new class of compounds the scientists developed can improve multiple aspects of metabolic syndrome. An increasingly common group of conditions that often occur together, metabolic syndrome includes type 2 diabetes, high cholesterol, fat buildup in the liver, and excess body fat, especially around the waist. This syndrome often leads to cardiovascular disease, the leading cause of death worldwide.
The study is published in the journal Nature Communications.
Testing one of the compounds referred to as SN-401, the researchers found it treats diabetes by improving the ability of the pancreas to secrete insulin and boosting the ability of other tissues to utilize that insulin to more effectively remove sugar from the bloodstream. In an effort to optimize the treatment, the researchers fine-tuned the compound — creating a class of related compounds — based on their studies of a key protein called SWELL1 (also LRRC8a). The gradual decline of this protein may have a central role in the development of diabetes and other aspects of metabolic syndrome.
“Our goal is to develop better therapies for cardiovascular disease, including diabetes and metabolic syndrome, which are major risk factors for worsening heart and vascular problems,” said senior author Rajan Sah, MD, PhD, an associate professor of medicine. “We have many treatments for diabetes, but even with those therapies, cardiovascular disease remains a leading cause of death among patients with type 2 diabetes. There is a need for new treatments that work differently from the current standard-of-care therapies.”
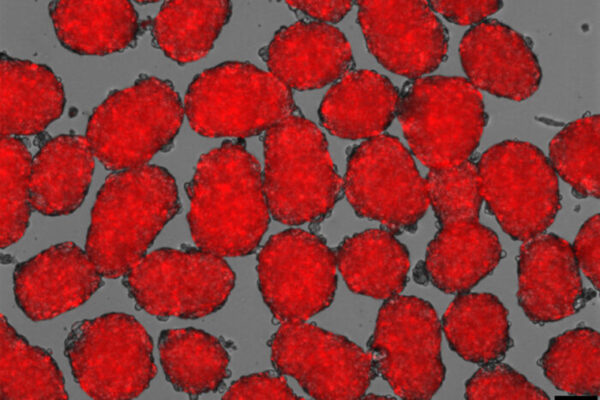
The protein Sah and his colleagues studied is called SWELL1 because of its role in sensing the size or volume of cells. Their new research reveals that the protein also helps to control insulin secretion from the pancreas and improve insulin sensitivity, including in skeletal muscle and adipose tissue, the body’s fat stores.
Surprisingly, the researchers showed that SWELL1 does both of these seemingly independent tasks because the protein has a previously unknown double life. It acts as a signaling molecule, turning on cellular tasks that govern how well cells use insulin and also facilitates the pancreas’ secretion of insulin into the bloodstream.
“This protein, SWELL1, has a sort of dual personality,” Sah said. “The compound binds to SWELL1 in a manner that stabilizes the protein complex so as to enhance expression and signaling across multiple tissues, including adipose, skeletal muscle, liver, the inner lining of blood vessels, and pancreatic islet cells. This restores both insulin sensitivity across tissue types and insulin secretion in the pancreas.”
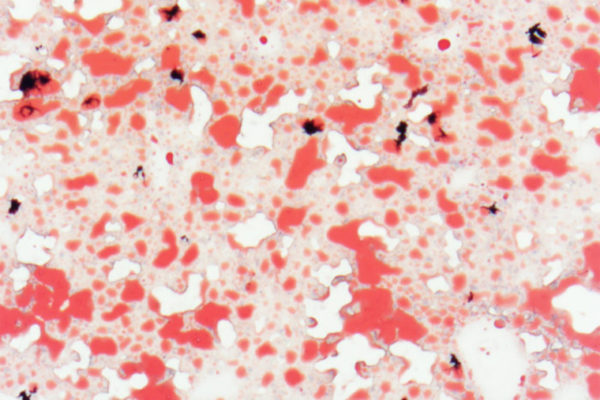
Sah and his colleagues showed that the SN-401 compound improved multiple aspects of metabolic syndrome in two groups of mice that each developed diabetes from different causes, one because of a genetic predisposition and the other due to a high-fat diet. In addition to improving insulin sensitivity and secretion, treatment with the compound also improved blood sugar levels and reduced fat buildup in the liver. Most of these studies were conducted with an injected form of the compound, but the researchers showed evidence that it also could be effective if taken by mouth.
The researchers further showed that the compound does not have a big impact on blood sugar in healthy mice, which is important for its potential as a future possible therapy. Current medications for diabetes can result in blood sugar levels that are too low. The evidence suggests that this compound does not lower blood sugar in situations when it doesn’t need to.
Sah worked with Washington University’s Office of Technology Management to patent the class of compounds and co-found a startup company called Senseion Therapeutics Inc., which is developing small molecule drugs that act on SWELL1. The company was first supported through funding from the university’s Leadership Entrepreneurship Acceleration Program (LEAP), and also recently received three Small Business Innovation Research (SBIR) grants totaling $4.5 million. SBIR grants are supported by the small business seed fund of the National Institutes of Health (NIH).
This work was supported by the National Institutes of Health (NIH), grant numbers P30CA086862, P30DK020579, T32GM008365, GM123496, GM128263, P30 DK056341, UL1 TR000448, T32 HL130357, R01DK115791, R01DK106009, R01DK126068, R01DK127080, R43 DK121598 and R44 DK126600; the John L. & Carol E. Lach Chair in Drug Delivery Technology; grants from the New York Stem Cell Foundation; a McKnight Foundation Scholar Award; a Rose Hill Innovator Award; a Sloan Research Fellowship; the Leadership Entrepreneurship Acceleration Program (LEAP) from the Skandalaris Center for Interdisciplinary Innovation and Entrepreneurship at Washington University in St. Louis; and the Roy J. Carver Trust, University of Iowa.
Gunasekar SK et al. Small molecule SWELL1 complex induction improves glycemic control and nonalcoholic fatty liver disease in murine type 2 diabetes. Nature Communications. Feb. 10, 2022.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, and currently is No. 4 in research funding from the National Institutes of Health (NIH). Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.