Investigators at Washington University School of Medicine in St. Louis conduct many clinical trials and translational research studies each year to develop and evaluate new ways of treating and diagnosing myriad types of diseases. Such research holds promise for improving the health of people living in St. Louis, across the state of Missouri and around the globe.
The School of Medicine has received a $61 million grant from the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) to support the infrastructure for developing and carrying out biomedical research studies. The funding supports Washington University’s Institute of Clinical and Translational Sciences (ICTS), which was established in 2007. The five-year grant renewal ensures that the ICTS will continue to serve as an engine of innovation in clinical and translational research across the region, with a focus on precision medicine, health equity and diversity.
The ICTS provides resources for investigators conducting clinical and translational research, including funding for personnel, training, laboratory space, scientific equipment and seed grants, to help speed the transition that can take a research discovery from the laboratory to the bedside, where newly developed therapies could help patients.
The ICTS supports almost 1,800 researchers at Washington University and about 530 investigators at other local and regional institutions, including collaborators at BJC HealthCare, Saint Louis University, the University of Health Sciences and Pharmacy in St. Louis, and the University of Missouri, Columbia.
Beyond the development of new treatments, the ICTS also is focused on nurturing engagement and collaboration with communities in St. Louis and making sure new discoveries are not only made but broadly implemented in clinical practice, so patients can benefit. In recent years, the ICTS also has proven instrumental in managing quick pivots so that the university can effectively address pressing global public health issues, such as the COVID-19 pandemic.
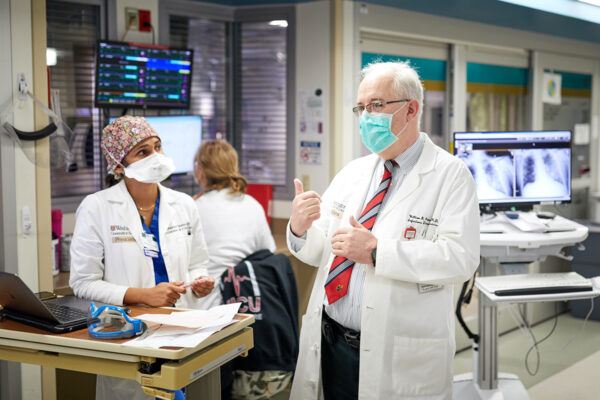
“The most important work that our ICTS has handled over the past five years was, without a doubt, our response to the COVID-19 pandemic,” said ICTS Director William G. Powderly, MD, the Dr. J. William Campbell Professor of Medicine, the associate dean for clinical and translational research, co-director of the Division of Infectious Diseases in the Department of Medicine, and the Larry J. Shapiro Director of the Institute for Public Health. “Through the ICTS, we have the infrastructure that can allow translational science to flourish and, at the same time, position us to respond well to a national emergency caused by brand-new infectious diseases.”
In particular, Powderly said that community advisers working with ICTS investigators played critical roles in helping Washington University implement COVID-19 vaccine clinical trials and, once such vaccines were broadly approved for the general public, vaccine delivery across the St. Louis region. Such advisers helped investigators understand the perspectives of the community, including the reluctance among some populations to getting vaccinated.
“Many times, people understand that if they participate in research, they won’t necessarily benefit directly themselves, but they still want to know what happened — what the study concluded,” Powderly said. “So, it’s important for us to cultivate relationships in the community so that we can tell the whole story, returning what we’ve learned to the people who helped us make these discoveries in the first place. We have a responsibility to make sure that results go back to patients and families so they can see the value of the research they or their loved ones are participating in.”
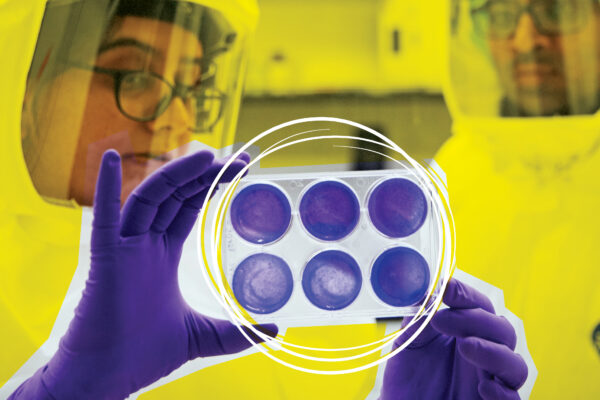
 Pictured are COVID-19 blood, urine and saliva samples stored at the Siteman Core Lab Services at the BJC Institute of Health at Washington University School of Medicine. The ICTS managed the collection of these samples from COVID-19 patients who volunteered to participate in research and the distribution of the samples to investigators across campus conducting COVID-19 research. (Photo: Matt Miller/School of Medicine)
Pictured are COVID-19 blood, urine and saliva samples stored at the Siteman Core Lab Services at the BJC Institute of Health at Washington University School of Medicine. The ICTS managed the collection of these samples from COVID-19 patients who volunteered to participate in research and the distribution of the samples to investigators across campus conducting COVID-19 research. (Photo: Matt Miller/School of Medicine)
With such ICTS goals in mind, Joyce Balls-Berry, PhD, an associate professor of neurology, is leading efforts to increase the inclusion of underrepresented communities in research on dementia, including Alzheimer’s disease. For reasons that remain unclear, Alzheimer’s dementia affects Black Americans at higher rates than white Americans. But most studies lack sufficient numbers of Black patients to be able to draw solid conclusions about how the disease might affect this population differently.
“It’s so important for Washington University researchers to understand concerns about the ethical conduct of research that the community might have and the work it takes to build trust and to serve as advocates for community health and wellness,” said Balls-Berry, who also leads the Health Disparities and Equity Core in the Knight Alzheimer Disease Research Center. “As an African American woman from St. Louis, this work is important to me because I want to make sure we are protective of our communities and not further marginalizing communities of color, who don’t often have a voice at the research table. We want to build these collaborations in a way that is sustainable and co-equal, meaning community members have a voice in these research projects from the beginning and throughout the process.”
To build on community engagement in the research process, infectious diseases specialist Elvin Geng, MD, a professor of medicine, also is working toward better dissemination of new knowledge gleaned from clinical trials, and improved implementation of the discoveries that are already available and can benefit patients today but are underused.
“In recent years in particular, we have developed amazing treatments and preventive interventions — such as vaccinations for many diseases, including COVID-19 — but the proportion of people who actually benefit from these innovations is far lower than it should be,” said Geng, who also is director of the Center for Dissemination & Implementation at the university’s Institute for Public Health. “It’s a sobering counterpoint to these innovations, but Americans receive maybe half of the health care they could benefit from. With this new ICTS funding, we would like to turn the scientific lens onto the problem of implementation itself — investigate and develop better ways to get the most effective health-care practices and treatments to everyone who can benefit from them.”
The Institute of Clinical and Translational Sciences is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH), grant number UL1 TR002345.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, and currently is No. 4 in research funding from the National Institutes of Health (NIH). Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.