Fragile X syndrome, the leading inherited cause of intellectual disability, is due to a genetic mutation that largely eliminates the fragile X protein, a critical element of normal brain development and function.
The fragile X protein modulates neuronal functions, including neurons within the so-called GABAergic system that regulates the activity of neural circuits. The protein’s absence throws that system off kilter, and so far, experimental therapies designed to reset the system by compensating for the missing protein’s functions have not been effective in clinical trials.
Now, researchers at Washington University School of Medicine in St. Louis have identified a previously unknown role for the fragile X protein in the GABAergic system. They have shown that the protein regulates the opening and closing of the GABA-A receptor in neurons from the brain’s memory center, thereby influencing how such neurons process information, a central part of learning and memory.
The findings, published May 17 in Cell Reports, indicate that the fragile X protein’s role is more complex than previously thought, and that finding effective therapies may depend on a more nuanced understanding of the myriad ways loss of this protein affects the brain.
“People think that since fragile X is related to the loss of a single protein, it is a simple disease that we can quickly understand and fix,” said senior author Vitaly A. Klyachko, PhD, a professor of cell biology and physiology. “But the reality is that the more we study, the more we understand it’s not simple at all. I think part of the reason why clinical trials fail may be because we don’t really understand what’s going on very well. It is possible that we need to fix more than one mechanism at the same time for patients to see any meaningful improvement.”
People with fragile X syndrome have intellectual or learning disabilities, social and behavioral problems, and characteristic physical features such as large ears and long faces. They also often are noted for their friendly dispositions. The condition affects about 1 in 7,000 males and 1 in 11,000 females, with males typically more severely affected. The fragile X gene is located on the X chromosome, so females inherit one good and one bad copy of the gene, but males have only the bad copy. There are no treatments that address the underlying cause.
The GABAergic system is based on the transmission of gamma aminobutyric acid (GABA) from one neuron to another. When it arrives, GABA binds to a receptor molecule and triggers a cascade of events in the receiving neuron that results in suppression of the activity of that neuron. An overactive GABAergic system puts people to sleep; an underactive one is linked to depression, anxiety and epileptic seizures.
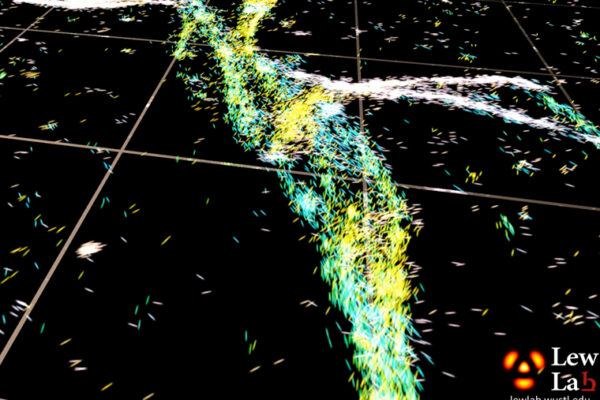
To better understand the role of fragile X protein in the GABAergic system, Klyachko and first author Pan-Yue Deng, MD, PhD, an associate professor of cell biology and physiology, studied neurons from the brains of mice with and without the fragile X protein. Specifically, they recorded the activity of key information-processing neurons controlled by the GABAergic system in the hippocampus, the brain’s learning and memory center. Such neurons sense the presence of GABA primarily by using the so-called GABA-A receptor.
The receptor is a channel that can open to allow negatively charged chloride ions to flow into the cell to modulate its activity. The researchers found that fragile X protein influences how much time the GABA-A receptor spends open and how much chloride it allows into the cell, thereby setting the baseline electrical charge inside the neuron. This baseline charge, in turn, affects the neuron’s ability to distinguish between multiple signals that arrive at nearly the same time, a critical mechanism of pattern separation essential for learning and memory formation.
“The fragile X protein directly interacts with receptors that play a major role in the way neurons process information,” Klyachko said. “This is an additional function for the fragile X protein, and it may be an important one. These neuronal receptors are everywhere, and they control many critical brain functions.”
But Klyachko cautions against assuming that these findings can be easily translated into therapies for people living with fragile X syndrome. The GABAergic system is complex, and small tweaks can have unexpected and far-reaching effects on brain function, he said.
“I think there is a very strong desire — an understandable one — to immediately translate each discovery into a clinical trial,” Klyachko said. “But if we don’t understand all of the functions this protein has and we try to go after one specific mechanism, it may destabilize the other ones, and the end result is that people don’t get better. An entirely different approach to treating this disease may be possible, but I think we need to first understand much more about how it works. This is just the first stepping stone in a new direction.”
Deng PY, Kumar A, Cavalli V, Klyachko VA. FMRP regulates GABAA receptor channel activity to control signal integration in hippocampal granule cells. Cell Reports. May 17, 2022. DOI: 10.1016/j.celrep.2022.110820
This work was supported by the National Institutes of Health (NIH), grant numbers R35NS111596, R01NS111719 and R35NS122260.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, and currently is No. 4 in research funding from the National Institutes of Health (NIH). Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.