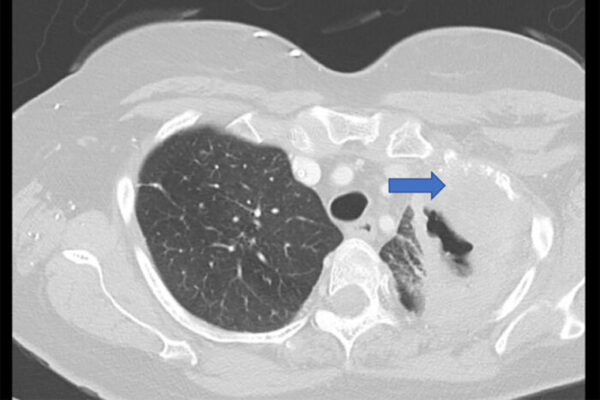
Regular postsurgical screening is critical for patients with lung cancer, the United States’ second most prevalent type of cancer and leading cause of cancer deaths. In cases involving early-stage non small cell lung cancer, up to half of patients will experience recurrence within the first two years after surgery.
For these reasons, guidelines by the National Comprehensive Cancer Network and other cancer groups recommend computed tomography (CT) scans every three to six months for patients who have had malignant lung tumors surgically removed. However, a new study by researchers at Washington University School of Medicine in St. Louis found no improvements in survival or recurrence rates among patients who followed the protocol, compared with those who were scanned every six months to one year.
“Our findings suggest that lung cancer treatment guidelines should consider less frequent surveillance imaging than current recommendations,” said the study’s senior author, Varun Puri, MD, a thoracic surgeon and professor of surgery. “Annual surveillance would simplify guidelines and may result in better, easier postoperative care for early-stage patients.”
The study is published Nov. 28 in the Journal of the National Cancer Institute.
Non-small cell lung cancer accounts for 84% of all lung cancer cases, according to the American Cancer Society, and the overall five-year survival rate is 25%.
The researchers focused on the first two years after surgery since that is when the risk of lung cancer recurrence is highest. After two to three years, cancer organizations typically recommend annual scans until the end of life.
“Scanning too frequently can be associated with unnecessary anxiety for patients and increased health-care costs,” said Puri, also a research member of Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital. “Patients who receive scans to check for recurrent cancer are understandably anxious, especially since it can take several days for results to be received. This phenomenon is sometimes called ‘scanxiety.’ It is obviously important to minimize scanxiety when it can be done safely.”
For the study, the researchers analyzed de-identified medical records in a database maintained by the U.S. Veterans Health Administration, the nation’s largest integrated health-care delivery system. The researchers examined information involving 6,171 patients with stage 1 non-small cell lung cancer who underwent surgery from Oct. 1, 2006, through Sept. 31, 2016. One patient group received scans every three to six months, and the other group every six to 12 months.
In all cases, more scans did not offer improved health, including among different tumor sizes, tumor stages and types of surgical procedures. Recurrence was observed in 22% of patients and did not differ based on the frequency of scanning. Similarly, overall survival remained the same between the two groups, with about 65% of patients surviving at least five years.
The average age of the patients was 67.5. The patients were predominantly male and white; however, statistical modeling controlled for different ages, genders and races.
“We found that certain patients had received more frequent CT scans, including patients who smoked and patients who had certain types of operations,” said the study’s first author, Brendan Heiden, MD, a surgical resident and research fellow at Washington University. “Conversely, we found that African-American patients received less frequent scans, which is a potentially concerning health disparity that warrants further research. Nonetheless, we were encouraged to find that patient outcomes were generally equivalent regardless of scan frequency.”
Heiden continued: “The VA treats a unique patient population that consists mostly of males with significant smoking histories. Therefore, we believe that our findings are most applicable to veterans with lung cancer. However, prior studies examining non-VA patient populations have found similar results to ours, suggesting that the results may apply more broadly to the general population. More research is needed.”
Heiden BT, Eaton Jr. DB, Chang S, Yan Y, Schoen MW, Thomas TS, Patel MR, Kreisel D, Nava RG, Meyers BF, Kozower BD, Puri V. Association between imaging surveillance frequency and outcomes following surgical treatment of early-stage lung cancer. Journal of the National Cancer Institute. Published Nov. 29, 2022. DOI: 10.1093/jnci/djac208.
This research was funded by National Institutes of Health (NIH) grant 5T32HL007776-25; and Veterans Administration grant 1I01HX002475-01A2.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,700 faculty. Its National Institutes of Health (NIH) research funding portfolio is the fourth largest among U.S. medical schools, has grown 54% in the last five years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,790 faculty physicians practicing at over 60 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.