Influenza viruses have an enormous impact in the U.S., with an estimated 25 million illnesses and 18,000 deaths in the 2022-23 flu season alone. However, the majority of virus particles are not infectious or are only partially infectious. How, then, do they become such a contagious and deadly virus?

Michael Vahey, an assistant professor of biomedical engineering at the McKelvey School of Engineering at Washington University in St. Louis, plans to investigate how two proteins on the surface of influenza virus influence how many viruses enter a cell and how infection spreads with a nearly $2 million five-year grant from the National Institutes of Health (NIH).
A viral particle cannot spread infection on its own — it must be absorbed by a cell where it can begin replicating and making copies of the viral genome and proteins. When two or more viruses enter into the same cell, they can sometimes work together to make new viruses more effectively. In this research, Vahey will look at how frequently this occurs and how this varies depending on the “stickiness” of the virus, or how well it is able to attach to the surface of new cells to infect them.
Vahey will study two viral proteins that are particularly important in this process: HA and NA. While HA binds to sugars on the surface of cells, NA helps to remove these sugars. The competition between these two proteins determines how well viral particles attach to new cells, Vahey said. This is the first phase of a viral invasion.
“If a virus is sticky, when it emerges from one infected cell, it may quickly attach to a new one nearby, creating a zone where the virus is very concentrated,” Vahey said. “In comparison, viruses that are less sticky may tend to spread out more, potentially infecting more cells, but with fewer viruses per cell. The central idea of our project is that the stickiness of the virus determines how frequently you have a co-infection and how readily a virus can complement itself.”
Vahey said that under normal circumstances, HA and NA are thought to be in balance for most human viruses.
“For a virus to spread efficiently, one can’t be dominant over the other,” he said. “But the balance can be thrown off when viruses enter into a new host species or when they mutate to avoid antibodies.”
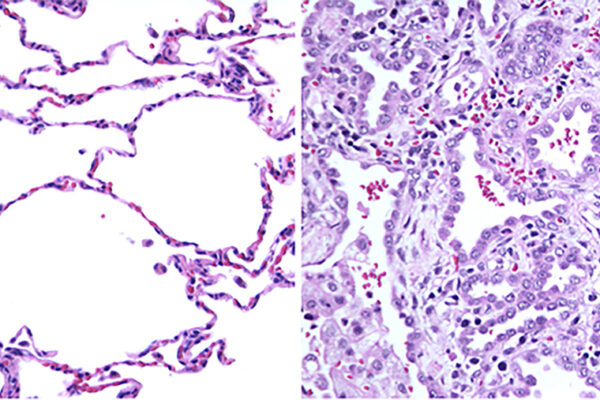
For the research, Vahey will collaborate with Steven L. Brody, MD, the Dorothy R. and Hubert C. Moog Professor of Pulmonary Diseases in Medicine and a professor of medicine and of radiology at Washington University School of Medicine, to use differentiated human tracheal cells that closely resemble the surface of the human airways. These cells possess motile cilia, tiny hair-like structures that beat rhythmically to sweep away the mucus produced by other cells. Cilia and mucus can also influence the way viruses spread throughout their environment.
“Our long-term goal is to be able to predict how a certain set of mutations in one protein or the other might manifest in the way that the virus is spreading through the human airways,” Vahey said. “I think that would put us in a better position to understand which combinations of mutations we need to be more concerned about and which may be less likely to cause problems.”
Originally published by the McKelvey School of Engineering