It’s not easy to distinguish between the dozens of subtypes of limb girdle muscular dystrophy — a rare, genetic muscle disease characterized by weakness in the hips and shoulders that causes difficulty walking and lifting the arms. Until now, determining the subtype has not been critical in caring for patients, because no specific treatments have been available. But gene therapies are on the horizon, and such therapies are targeted to specific genetic variants, so pinpointing the genetic roots of each patient’s disease has taken on a new importance.
In new research, a team at Washington University School of Medicine in St. Louis has developed an approach that could help doctors make more precise diagnoses. The study is published June 15 in The Journal of Clinical Investigation.
Hundreds of genes are associated with limb girdle muscular dystrophy. While genetic testing may identify a handful of rare genetic variants in each patient with the condition, there’s no way to know without painstaking, time-consuming additional experiments which, if any, of those variants is responsible for a patient’s symptoms. Unfortunately, no comprehensive catalog exists yet of all the variants of all the genes linked to limb girdle muscular dystrophy, and whether each of those variants can cause disease or is harmless.
“There are people emailing me all the time saying, ‘I have this variant. Am I eligible for this experimental therapy?’ and much of the time I don’t have an answer,” said co-author Conrad “Chris” Weihl, MD, PhD, a professor of neurology. Weihl is chief of the neuromuscular diseases section and treats people with muscular dystrophy at Barnes-Jewish Hospital. “These patients are in limbo. We can’t get them into clinical trials until they have a diagnosis. More than half of all patients with limb girdle muscular dystrophy are in this position. It’s critical that we resolve their diagnoses so we can get them access to necessary therapies as soon as they become available.”
Weihl and colleagues at Washington University have taken an important step toward creating a catalog that could help resolve inconclusive diagnoses. For one gene commonly involved in the disease, the researchers created the protein that would be made from that gene’s instructions. Then, they made every possible protein variant that could be formed by swapping out one amino acid for another, analyzed the functions of the variants and classified each as harmful or benign. Now, if a patient has a variant of this one gene, doctors can determine its pathogenicity simply by looking up the variant in the catalog. In principle, the same approach could be used to resolve variants of unknown significance for many other genes associated with limb girdle muscular dystrophy, vastly simplifying and speeding up the process of diagnosing this complex disease.
“People conflate knowing that there is a variant with knowing the cause of a disease,” said corresponding author Gabriel Haller, PhD, an assistant professor of neurosurgery. “That isn’t necessarily the case. In this study, most of the variants of unknown significance turned out to be benign. If you find a variant but you don’t know its significance, you haven’t figured out the answer.”
Resolving variants of unknown significance is particularly beneficial to members of underrepresented groups. Genetic databases are dominated by people of western European background and reflect the genetic diversity found in that population. People of other backgrounds are more likely to carry genetic variations that have no match in reference databases and thus get the label “variant of unknown significance.”
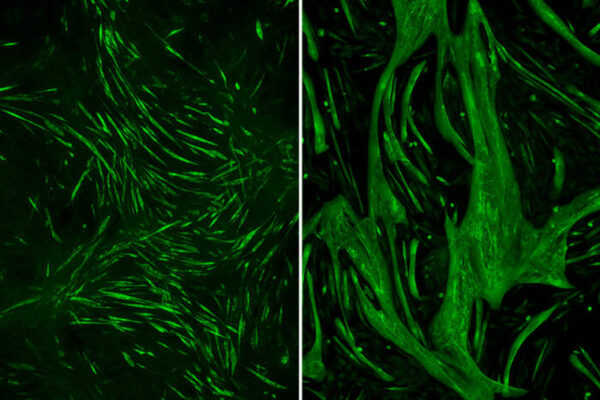
For this study, the researchers did a comprehensive analysis of sarcoglycan beta, one of the genes most often linked to limb girdle muscular dystrophy. Sarcoglycan beta forms a complex with three other proteins on the surface of muscle cells. For muscles to contract effectively, the complex must form properly and in the right place on the cell. First author Chengcheng Li, PhD, a staff scientist in Weihl’s lab, created all 6,340 possible variants of sarcoglycan beta protein. Then, she assessed where each variant protein was located on muscle cells, using a fluorescent antibody. Those variants capable of forming the correct complex at the correct spot — in other words, variants with normal functional activity — fluoresced brightly. Those that failed to form the complex properly or were located at the wrong place — i.e., less functional variants — fluoresced more dimly.
The correlation was perfect. All variants known to cause disease scored low in functional activity, while all known benign variants scored high. Not only that, the degree of functional activity correlated with severity of disease. People with the most severe symptoms of limb girdle muscular dystrophy may need to start using wheelchairs as young as age 7, while people with milder symptoms may not need one until decades later, if ever. In the study, variants with lower functional activity more often appeared in patients with more severe symptoms.
“Twenty percent of the variants of unknown significance turned out to be pathogenic, which means they could be amenable to potential therapies,” Weihl said. “My dream is that one day we’ll be able to give people a genetic test report that says, ‘You have this variant, and it’s amenable to this type of therapy,’ and we can start them on the best therapy right away. Or we tell them, ‘Your variant is benign,’ and we keep looking until we find the variant that is responsible for the patient’s disease.”
Li C, Wilborn J, Pittman S, Daw J, Alonso-Pérez J, Díaz-Manera J, Weihl CC, Haller G. “Comprehensive functional characterization of SGCB coding variants predict pathogenicity in limb-girdle muscular dystrophy type R4/2E.” The Journal of Clinical Investigation. June 15, 2023. DOI: 10.1172/JCI168156
Funding for this project was provided by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, grant number CDI-II-2022-1015; and by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (NIH), grant number R21AR078942.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.