We’ve come a long way in the 43 months since March 2020, when the World Health Organization declared a global pandemic in the wake of the SARS-CoV-2 virus outbreak, but still we can’t shake it. Long COVID remains a mystery and a new variant has popped up. A renewed booster shot is now available, and nearly four years later, masking remains an important part of the public health conversation.
But there is reason for optimism, thanks to a multidisciplinary team of Washington University in St. Louis researchers. This summer, researchers from the School of Medicine and the McKelvey School of Engineering published two papers announcing the development of two new devices that ultimately could go a long way in dealing with this virus — and ultimately viruses that could cause future pandemics.
“One of the silver linings of the pandemic is that it forced collaborations between disciplines that otherwise would not have taken place.”
Rajan Chakrabarty
The first was an air quality monitor that can detect SARS-CoV-2 in public spaces, the second a breathalyzer that can provide a quicker diagnosis of individuals. And both happened because of a collaboration between WashU scientists who had never met in person and wouldn’t do so — because of social distancing — for more than a year.
“One of the silver linings of the pandemic,” says Rajan Chakrabarty, the Harold D. Jolley Career Development Associate Professor of energy, environmental & chemical engineering in McKelvey Engineering, “is that it forced collaborations between disciplines that otherwise would not have taken place.”
Chakrabarty recalls he had begun to pivot his team to modeling how fast the virus was transmitting when he got an email in July 2020 from John Cirrito, professor of neurology at the School of Medicine. The National Institutes of Health (NIH) had put out a call for “radical approaches” to virus detecting devices, specifically asking for research “outside the typical NIH domain,” Chakrabarty says. “Engineers typically do not apply for NIH grants.”
It was one of those fortunate convergences of talent, hard work, ingenuity — and timing. Cirrito and Carla Yeude, associate professor of psychiatry, had a decade of work developing a biosensor to detect amyloid beta and other Alzheimer’s disease-related proteins in the brains of mice. They had access to a nanobody, an antibody from llamas, that was sensitive to the virus. Chakrabarty, an expert on aerosols engineering, recruited Joseph Puthussery, a postdoctoral research associate in his lab who had expertise in building real-time instruments to measure the toxicity of air. The collaboration was on. By late fall 2020, they had the funding through the NIH’s RADx-Rad program.
“Once we had the money, the work was nonstop,” Chakrabarty says.
The devices
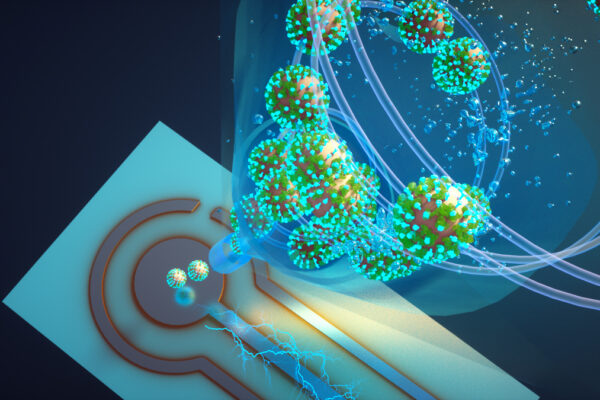
The real-time air quality monitor can detect any of the SARS-CoV-2 virus variants in a room in about 5 minutes. The inexpensive, proof-of-concept device could be used in hospitals and health-care facilities, schools and public places to help detect SARS-CoV-2 and potentially monitor for other respiratory virus aerosols, such as influenza and respiratory syncytial virus (RSV).
“There is nothing at the moment that tells us how safe a room is,” Cirrito says. “If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real time, or every 5 minutes, if there is a live virus in the air.”
Air monitor can detect COVID-19 virus variants in about 5 minutes
Read the original story about the air quality monitor here.
The breathalyzer device requires only one or two breaths and provides results in less than a minute. And when new strains of COVID-19 or other airborne pathogenic diseases arise, such devices could be used not only to screen individuals at doctors’ offices but also at public events. The breath test also has potential to help prevent outbreaks in situations where many people live or interact in close quarters — for example, aboard ships, in nursing homes, in residence halls at colleges and universities, or on military bases.
“With this test, there are no nasal swabs and no waiting 15 minutes for results, as with home tests,” Chakrabarty says. “A person simply blows into a tube in the device, and an electrochemical biosensor detects whether the virus is there. Results are available in about a minute.”
Scientists develop breath test that rapidly detects COVID-19 virus
Read the original story about the breathalyzer device here.
What’s next
Eventually, the team met in person, but it took about a year. Now, Chakrabarty says, they work independently but speak almost daily. “Our two papers created a lot of splash,” Chakrabarty says. “Since they came out this summer, our days have been filled with meetings with potential investors and nonprofits. Even the public. We receive emails from people who just want these devices out there.”
“We have these prototypes. Now, our focus is on how to best address the needs of the public.”
Rajan Chakrabarty
But Congress has pulled back on COVID funding, so now, Chakrabarty says, the interest is to develop a “multiplex device that can simultaneously detect COVID or influenza or even RSV, and that’s the angle we’re taking.”
Chakrabarty hopes to have devices that can detect multiple viruses and pathogens ready for public use within two years. That may seem like a long time, but he’s amazed at how far they’ve come already. “It’s been an interesting evolution,” Chakrabarty says. “We have these prototypes. Now, our focus is on how to best address the needs of the public.”
Still, the speed with which these devices came about amazes the engineer himself. “Rarely in a scientist’s life, do you come across ‘aha’ moments,” he says. “And although we assimilated novel technologies, we did not have a template to build upon. We had to start from scratch — the last three years have been crazy.”
The work of Beth Miller, Jim Dryden and Tamara Bhandari contributed to this piece.