Every day in the U.S. in 2018, motor vehicle crashes killed more than 20 people over age 65 and injured almost 700. Older adults are the most responsible drivers of any age group — they tend to obey speed limits and avoid driving at night and in bad weather, for example — but the physical changes of aging put them at risk of accidents.
Researchers at Washington University School of Medicine in St. Louis have received three grants totaling more than $10 million to study the factors that contribute to deterioration in driving skills in older adults and to determine ways to identify people whose driving skills have begun to decline or are on the verge of slipping. The ultimate goal is to understand who’s at risk behind the wheel so doctors can intervene to help them preserve their skills or safely adapt to new limitations.
“Driving is an integral part of the American identity,” said Ganesh Babulal, assistant professor of neurology. Babulal is the principal investigator on two of the grants and a co-principal investigator on the third. “For the next three decades, there’s going to be massive growth of the aging population, and driving — not autonomous vehicles or ride-sharing, but driving yourself — will continue to be the primary method of transportation.”
Two of the grants — one from the BrightFocus Foundation and the other from the National Institutes of Health (NIH) — support studies to determine whether driving changes can identify people with mild and very mild cognitive impairment, and maybe even identify people in the earliest, presymptomatic stage of Alzheimer’s disease.
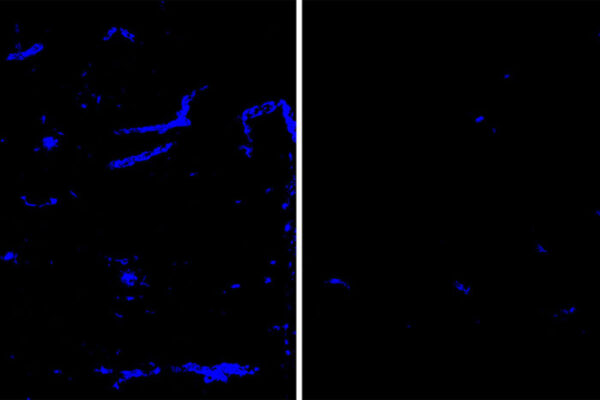
Alzheimer’s affects one in 10 people over age 65. The disease develops slowly, beginning with the buildup of protein plaques in the brain two decades or more before cognitive symptoms arise.
“Alzheimer’s disease affects more than just thinking and memory,” said Catherine Roe, associate professor of neurology and a co-principal investigator on the NIH grant. “It affects your reaction time, eyesight, strength and gait, mood. All of these factors also are related to driving, so it’s not unreasonable to suppose that you might see some effect on driving even before cognitive symptoms are apparent.”

In 2015, Roe and Babulal started studying how Alzheimer’s disease affects driving under real-world conditions. They designed the Driving Real-World In-Vehicle Evaluation System (DRIVES) chip to monitor how people drive in their own cars and their own neighborhoods over long periods of time. The chip plugs into a port, under the dashboard, that auto mechanics use to evaluate cars’ computer systems. The chip sends pulses of data every 30 seconds, stamped with the time and the car’s location. When a driver brakes hard, accelerates suddenly or the vehicle hits something, the chip shares that information with the researchers.
Roe and Babulal have been following some drivers for five years. They have found that the driving habits of people with Alzheimer’s disease deteriorate over time. Now, they want to know whether the inverse is also true: Can driving data be used to help identify people with Alzheimer’s? The researchers plan to combine driving data with measurements of molecular signs of Alzheimer’s and factors such as age and gender to build a model that can identify people with early Alzheimer’s — with or without cognitive symptoms — based primarily on their driving habits.
“Right now, early Alzheimer’s disease can be identified using cerebrospinal fluid or brain scans, but most people are still diagnosed only after they show unmistakable signs of cognitive decline,” Roe said. “If we could use driving behaviors to help us figure out who might have underlying Alzheimer’s, that would be an economical, naturalistic way to identify people with mild symptoms or even presymptomatic people.”
Babulal is also the principal investigator on a third grant, also from the NIH, focusing on the impact of depression on driving. Like Alzheimer’s, depression is a common ailment of the elderly and also has been linked to changes in driving behavior. But how depression and Alzheimer’s interact to affect driving is not well understood.
“Depression and Alzheimer’s impact memory and thinking in similar ways,” Babulal said. “A lot of Alzheimer’s studies screen out people with depression because it makes the data noisy. We wanted to embrace the noise. We are very carefully defining what is depression and what is cognition so that we can try to disentangle the effects of depression and Alzheimer’s on driving. I suspect that people who have both depression and Alzheimer’s are at the highest risk for deterioration of their driving skills and that we really need to pay attention to them in terms of driver safety.”
Babulal and Roe are looking for participants age 65 or older to participate in their driving studies. Participants need to be able to come to the School of Medicine to receive the DRIVES chip and undergo a clinical assessment and other exams for molecular signs of Alzheimer’s disease. People outside the St. Louis area can participate remotely, but they will need to be able to come in for regular assessments. For more information, call 314-747-1474, email drivesproject@wustl.edu or visit https://roelab.wustl.edu/interested-in-participating/.
Washington University School of Medicine’s 1,500 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, ranking among the top 10 medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.