Researchers at Washington University School of Medicine in St. Louis have received a grant from the National Institutes of Health (NIH) to establish a Pediatric Center of Excellence in Nephrology. The center’s physician-scientists will create high-definition molecular reference maps showing genetic details of normal and diseased kidneys during various stages of childhood growth and development. The center’s team also will launch related educational programs to draw new researchers into the field.
Kidney problems in children can range from short-term treatable disorders to chronic illnesses with devastating long-term consequences, including kidney failure, which requires dialysis treatment and often a kidney transplant. Common causes of kidney disease include birth defects, hereditary diseases, immunologic injury, infections and the consequences of other systemic problems, such as diabetes and hypertension. Chronically ill children with kidney disease may spend more time in the hospital, incur larger health-care costs and have a higher risk of death compared with pediatric patients hospitalized for other chronic conditions, research suggests.
“The development of effective methods for early detection and severity measurement of renal disease in children is lagging in part due to a lack of knowledge of physiological and pathological changes that occur as the kidney matures,” said co-principal investigator Vikas Dharnidharka, MD, director of the Division of Pediatric Nephrology, Hypertension & Pheresis in the Department of Pediatrics at the School of Medicine. “The molecular blueprints generated by our initiative will dramatically enhance our ability to design effective approaches to intervene and prevent kidney dysfunction.”
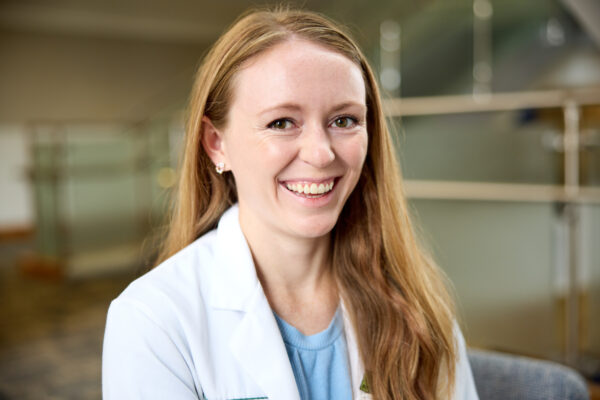
Dharnidharka, the Alexis F. Hartmann Sr., MD, Professor of Pediatrics and vice chair of clinical investigations in the Department of Pediatrics, is also co-medical director of the Pediatric Kidney Transplant Program at St. Louis Children’s Hospital, where he treats patients. Known nationally for expertise in diagnosing and treating kidney disease, Washington University pediatric specialists have led St. Louis Children’s to become a major referral center for children with kidney disease.
Sanjay Jain, MD, PhD, a professor of medicine in the Department of Medicine’s Division of Nephrology, will serve as co-principal investigator and project leader for the initiative. Jain, an investigator with the school’s Center of Regenerative Medicine, researches the biology of the kidney and lower urinary tract stem cells, with an emphasis on their potential to differentiate or remain stable in healthy and diseased states.
His lab explores how kidneys form, how they connect to the bladder, and how their cellular and molecular composition changes across the life span. His other NIH projects include the Kidney Precision Medicine Initiative and the Kidney Single Cell and Spatial Molecular Atlas Project as part of Human Biomolecular Atlas Project, with funding through the NIH Common Fund, the Kidney Precision Medicine Project and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
The Center of Excellence awards are funded through a highly competitive, five-year selection process administered by the NIDDK. Only three such projects are awarded funding each cycle.
The initiative’s leaders will manage an annual pilot project program and various educational initiatives, including an annual research symposium, an eight-week summer internship program and a visiting lecture program, all designed to draw new researchers to the field. Funding for the programs runs through June 2027.
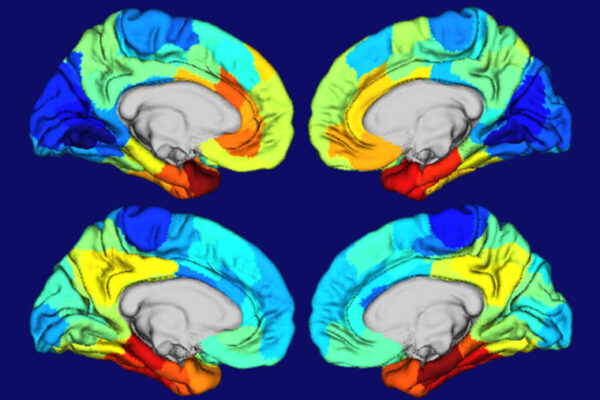
The investigators will analyze healthy and diseased samples from pediatric kidneys using single cell and spatial transcriptomics, a molecular profiling method that allows scientists to precisely measure and map where gene activity is occurring within a single cell or group of cells. By comparing how gene expression and cellular functions change during healthy development and disease progression, investigators hope to pinpoint changes that play a role in making and maintaining healthy kidneys and those that contribute to disease.
“Our goal is to detail the genetic and cellular mechanisms of childhood kidney disease and its progression to aid development of new diagnostic tests, improved drugs, unique personalized therapies and other clinical improvements that will help us limit or even cure genetic or acquired kidney disorders,” Jain said.
Other Washington University co-investigators are Michael Rauchman, MD, the Chromalloy Professor of Renal Diseases in Medicine; and Joseph Gaut, MD, PhD, the Ladenson Professor of Pathology & Immunology. The multidisciplinary team also includes co-investigators Gloria Pryhuber, MD, a neonatologist from the University of Rochester, and Michael Eadon, MD, a nephrologist from Indiana University.
The Washington University Pediatric Center of Excellence in Nephrology is supported by the National Institute of Diabetes and Digestive and Kidney Diseases, project number 1P50DK133943-01
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,700 faculty. Its National Institutes of Health (NIH) research funding portfolio is the fourth largest among U.S. medical schools, has grown 54% in the last five years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,790 faculty physicians practicing at over 60 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.