A new drug has been approved by the Food and Drug Administration (FDA) for a rare, inherited form of amyotrophic lateral sclerosis (ALS), a paralyzing neurological disease. Known as tofersen, the drug has been shown to slow progression of the deadly disease. International clinical trials of tofersen, developed by the global biotechnology company Biogen Inc., were led by a neurologist at Washington University School of Medicine in St. Louis.
Tofersen, also known by the brand name Qalsody, is designed for ALS patients whose disease is caused by mutations in the gene SOD1. In the phase 3 clinical trial, the drug reduced molecular signs of disease and curbed neurodegeneration in the first six months of use. Over longer time frames, some participants experienced a stabilization of muscle strength and control.
The drug is approved under the accelerated approval pathway, under which FDA may approve drugs for serious conditions where there is an unmet medical need and a drug is shown to have an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients.
“ALS is a devastating and deadly disease,” said Timothy M. Miller, MD, PhD, the David Clayson Professor of Neurology at Washington University and the principal investigator of the tofersen clinical trials. “The majority of patients experience a rapid and relentless decline in muscle strength that leads to death within five years. Up to now, we haven’t had any treatments that substantially change the course of the disease. This FDA decision means that people with SOD1 ALS now have access to a treatment that appears to slow down the neurodegenerative disease process and helps preserve motor function. This gives me hope that this could have a positive impact on the quality of life for people living with this rare form of ALS.”
About 20,000 people in the United States are living with ALS, also known as Lou Gehrig’s disease. The condition kills the nerve cells that control the muscles needed for moving around and for carrying out vital activities such as eating and breathing. About 2% of ALS cases are caused by mutations in the SOD1 gene.
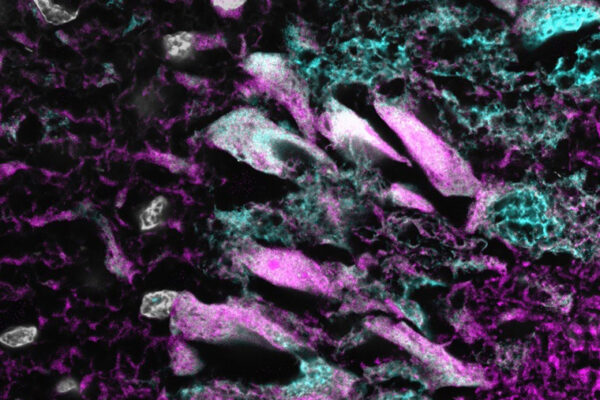
Miller, also co-director of the School of Medicine’s ALS Center, first began searching for therapies for ALS as a postdoctoral researcher two decades ago. He saw an opening in the rare cases of ALS caused by mutations in SOD1. The vast majority of ALS cases occur seemingly at random, in people with no clear risk factors, and scientists still have little understanding of why such cases arise. In contrast, the source of the problem in SOD1 ALS is well-known: mutant SOD1 protein is toxic to neurons. At the time Miller began studying SOD1 ALS, scientists were just beginning to explore a new technology for reducing disease-causing proteins using modified DNA molecules known as antisense oligonucleotides. Such molecules interfere with the genetic instructions for building proteins and can be designed to target specific problematic proteins such as SOD1.
After antisense oligonucleotides showed promise in animal studies of SOD1 ALS, Miller — along with Merit Cudkowicz, MD, the director of the Sean M. Healey & AMG Center for ALS at Massachusetts General Hospital — co-led the first clinical trial of an antisense oligonucleotide in the central nervous system. The phase 1 trial in patients with SOD1 ALS demonstrated that an antisense oligonucleotide could be safely delivered directly into the cerebrospinal fluid that bathes the brain and spinal cord. The experimental drug used in that first trial turned out to be less than ideal for treating ALS, but the trial yielded valuable insights into the biology of SOD1 ALS and the potential of antisense oligonucleotides to treat it. Miller and colleagues — including collaborators at Ionis Pharmaceuticals and Biogen — developed new and improved antisense oligonucleotides that resulted in tofersen.
The six-month phase 3 trial of tofersen — known as the VALOR trial — showed that the drug reduces levels of SOD1 and also neurofilament light protein, a molecular marker of neurological damage. At the end of the placebo-controlled part of the study, participants were offered the option to receive tofersen as part of an open-label extension that will last up to 4½ years.
“It took some time before we saw an effect, but after about six months on the drug, a number of patients stabilized, and some have exhibited objective improvements in muscle strength and function,” said Robert Bucelli, MD, PhD, a professor of neurology and co-director of the university’s ALS Center. As the Washington University site leader for the tofersen clinical trials, Bucelli has cared for 24 participants in tofersen-related studies. “As a physician caring for many ALS patients, the degree of benefit exhibited by some patients treated with tofersen has been impressive. ALS patients normally experience a relentless, progressive decline. These results have transformed my perspective on ALS as a treatable disorder.”
Tofersen will only benefit the small fraction of ALS patients whose disease is caused by SOD1 mutations. But the success of this approach shows that it is possible to change the course of a disease once thought to be untreatable.
“My whole career has been built on the assumption that ALS is a treatable disorder,” Miller said. “It’s all about finding the right therapy. Tofersen appears to be the right therapy for SOD1 ALS. Now we have to find the right therapy for other forms of ALS.”
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.