Anesthesiologist Michael S. Avidan, MBBCh, reproductive biologist Sarah K. England, PhD, and neurologist Timothy Miller, MD, PhD, all of Washington University School of Medicine in St. Louis, have been elected to the National Academy of Medicine, a part of the National Academy of Sciences. Membership in the organization is one of the highest honors in the fields of health and medicine in the United States.
They are among 90 regular members and 10 international members whose election to the National Academy of Medicine was announced Monday, Oct. 9. Current members of the organization elect new members based on their contributions to advancing public health, health care and medical science. All members volunteer time to serve on committees examining a broad range of health-policy issues.
Michael S. Avidan, MBBCh
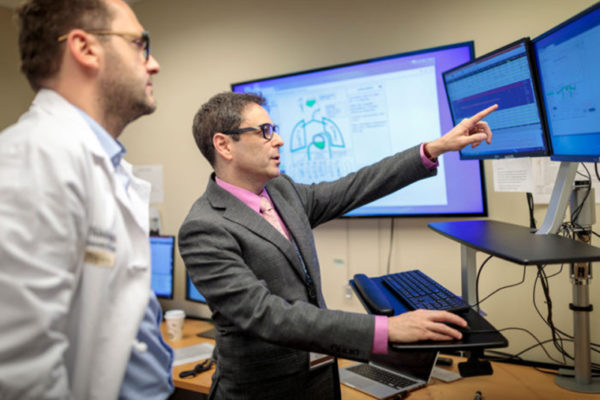
Avidan is the Dr. Seymour and Rose T. Brown Professor of Anesthesiology, head of the Department of Anesthesiology at Washington University and anesthesiologist-in-chief at Barnes-Jewish Hospital. He specializes in investigating the effectiveness of interventions to prevent neurologic complications associated with surgery and general anesthesia.
From 2006 through 2012, he led two large clinical trials in the U.S. and Canada that focused on the prevention of intraoperative awareness, when patients regain consciousness to the point where they retain memories of surgery. The findings, which were published in two highly cited papers in The New England Journal of Medicine, have had a major impact on monitoring techniques now widely employed during surgery.
Avidan’s other key research activities have included studies that led to the recognition that surgery and anesthesia are unlikely to hasten the onset of dementia or accelerate cognitive decline in patients with Alzheimer’s disease. He also implemented a telemedicine “control tower” at Barnes-Jewish Hospital that takes advantage of artificial intelligence and machine-learning techniques to allow anesthesia clinicians to monitor anesthesia care in many operating rooms simultaneously and provide expert assistance to troubleshoot rare but potentially life-threatening complications that arise during or around the time of surgery. Currently, Avidan is a co-principal investigator for the 12,500-patient, multicenter THRIVE trial, which aims to determine which type of general anesthesia results in the best patient experience and recovery.
Avidan is also a co-director of the Center for Perioperative Mental Health and a co-director of the Anesthesiology Postdoctoral Research Training Program.
Sarah K. England, PhD
England is the Alan A. and Edith L. Wolff Professor of Medicine and vice chair of research in the Department of Obstetrics & Gynecology. She also directs the Center for Reproductive Health Sciences. She specializes in understanding uterine function during pregnancy for people undergoing normal labor and delivery and those experiencing preterm labor. In particular, England’s research aims to uncover the molecular underpinnings of uterine function with the goal of developing therapeutics to support healthy labor and delivery.
A noted reproductive biologist, England is also a professor of obstetrics & gynecology and of cell biology & physiology, and a member of the Center for Women’s Health Engineering in the McKelvey School of Engineering. Her research is focused on the role of sodium and potassium channels in the muscle layer of the uterus, with the aim of developing therapeutics to stop premature uterine contractions that can cause maternal and fetal health complications and death.
England’s lab also studies oxytocin, a hormone used to induce or increase labor in nearly half of the women who give birth in the United States. Specifically, her lab studies the effects of different genetic variants in the oxytocin receptor on uterine function, also with the goal of developing therapeutics. Additionally, England’s research aims to determine if disruptions in maternal circadian rhythms — the body’s internal clock regulating sleep and activity cycles — are associated with preterm birth and if socially disadvantaged women are disproportionately affected.
Timothy Miller, MD, PhD
Miller is the David Clayson Professor of Neurology, a co-director of the amyotrophic lateral sclerosis (ALS) Center and vice chair for research in the Department of Neurology. He is recognized for developing a new approach to treating neurodegenerative diseases based on using a modified form of DNA known as antisense oligonucleotides.
Many neurodegenerative diseases are caused by excessively high levels or defective forms of specific proteins. Antisense oligonucleotides can be specially designed to target an unwanted protein and prevent the body from making more of it. Miller applied antisense technology to a form of ALS caused by a mutated form of the SOD1 gene. After the approach showed promise in animal studies, Miller led a phase 3 clinical trial that showed that targeting this gene with an experimental drug improves molecular signs of disease in people, and may help stabilize muscle strength and control. The drug, known as tofersen (brand name Qalsody), was approved by the Food and Drug Administration as a therapy for SOD1 ALS this year.
Miller’s work on antisense oligonucleotides also has contributed to a compound that is being studied for its potential to treat neurological diseases involving the tau protein, such as Alzheimer’s disease. The approach he developed is broadly applicable to many neurologic diseases.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.