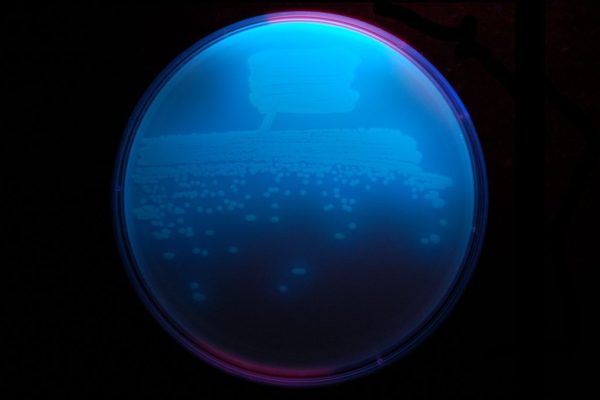
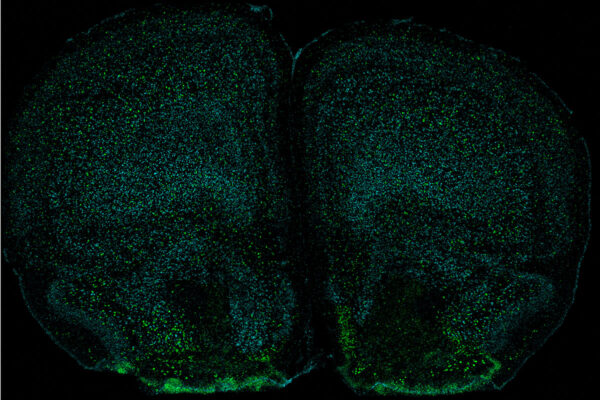
Shown above are two different 3D views of TetX7 (green), a tetracycline-destroying enzyme that causes resistance to all tetracycline antibiotics (the small multicolored molecule in the center). Researchers at Washington University in St. Louis and the National Institutes of Health (NIH) have found that genes that confer the power to destroy tetracyclines are widespread in bacteria that live in the soil and on people. (Video: Timothy Wencewicz)
The latest generation of tetracyclines — a class of powerful, first-line antibiotics — was designed to thwart the two most common ways bacteria resist such drugs. But a new study from researchers at Washington University in St. Louis and the National Institutes of Health (NIH) has found that genes representing yet another method of resistance are widespread in bacteria that live in the soil and on people. Some of these genes confer the power to destroy all tetracyclines, including the latest generation of these antibiotics.
However, the researchers have created a chemical compound that shields tetracyclines from destruction. When the chemical compound was given in combination with tetracyclines as part of the new study, the antibiotics’ lethal effects were restored.
The findings, available online in Communications Biology, indicate an emerging threat to one of the most widely used classes of antibiotics — but also a promising way to protect against that threat.
“We first found tetracycline-destroying genes five years ago in harmless environmental bacteria, and we said at the time that there was a risk the genes could get into bacteria that cause disease, leading to infections that would be very difficult to treat,” said co-senior author Gautam Dantas, professor of pathology and immunology and of molecular microbiology at Washington University School of Medicine in St. Louis. “Once we started looking for these genes in clinical samples, we found them immediately. The fact that we were able to find them so rapidly tells me that these genes are more widespread than we thought. It’s no longer a theoretical risk that this will be a problem in the clinic. It’s already a problem.”
In 2015, Dantas, also a professor of biomedical engineering, and Timothy Wencewicz, associate professor of chemistry in Arts & Sciences at Washington University, discovered 10 different genes that each gave bacteria the ability to dice up the toxic part of the tetracycline molecule, thereby inactivating the drug. These genes code for proteins the researchers dubbed tetracycline destructases.
But they didn’t know how widespread such genes were. To find out, Dantas and first author Andrew Gasparrini – then a graduate student in Dantas’ lab – screened 53 soil, 176 human stool, two animal feces, and 13 latrine samples for genes similar to the 10 they’d already found. The survey yielded 69 additional possible tetracycline-destructase genes.
Then they cloned some of the genes into E. coli bacteria that had no resistance to tetracyclines and tested whether the genetically modified bacteria survived exposure to the drugs. E. coli that had received supposed destructase genes from soil bacteria inactivated some of the tetracyclines. E. coli that had received genes from bacteria associated with people destroyed all 11 tetracyclines.
“The scary thing is that one of the tetracycline destructases we found in human-associated bacteria – Tet(X7) – may have evolved from an ancestral destructase in soil bacteria, but it has a broader range and enhanced efficiency,” said Wencewicz, who is a co-senior author on the new study. “Usually there’s a trade-off between how broad an enzyme is and how efficient it is. But Tet(X7) manages to be broad and efficient, and that’s a potentially deadly combination.”
In the first screen, the researchers had found tetracycline-destructase genes only in bacteria not known to cause disease in people. To find out whether disease-causing species also carried such genes, the scientists scanned the genetic sequences of clinical samples Dantas had collected over the years. They found Tet(X7) in a bacterium that had caused a lung infection and sent a man to intensive care in Pakistan in 2016.
Tetracyclines have been around since the 1940s. They are one of the most widely used classes of antibiotics, used for diseases ranging from pneumonia, to skin or urinary tract infections, to stomach ulcers, as well as in agriculture and aquaculture. In recent decades, mounting antibiotic resistance has driven pharmaceutical companies to spend hundreds of millions of dollars developing a new generation of tetracyclines that is impervious to the two most common resistance strategies: expelling drugs from the bacterial cell before they can do harm, and fortifying vulnerable parts of the bacterial cell.
The emergence of a third method of antibiotic resistance in disease-causing bacteria could be disastrous for public health. To better understand how Tet(X7) works, co-senior author Niraj Tolia, a senior investigator at the National Institute of Allergy and Infectious Diseases at the NIH, and co-author Hirdesh Kumar, a postdoctoral researcher in Tolia’s lab, solved the structure of the protein.
“I established that Tet(X7) is very similar to known structures but way more active, and we don’t really know why because the part that interacts with the tetracycline rings is the same,” Kumar said. “I’m now taking a molecular dynamics approach so we can see the protein in action. If we can understand why it is so efficient, we can design even better inhibitors.”
Wencewicz and colleagues previously designed a chemical compound that preserves the potency of tetracyclines by preventing destructases from chewing up the antibiotics. In the most recent study, co-author Jana L. Markley, a postdoctoral researcher in Wencewicz’s lab, evaluated that inhibitor against the bacterium from the patient in Pakistan and its powerful Tet(X7) destructase. Adding the compound made the bacteria two to four times more sensitive to all three of the latest generation of tetracyclines.
“Our team has a motto extending the wise words of Benjamin Franklin: ‘In this world nothing can be said to be certain, except death, taxes and antibiotic resistance,’” Wencewicz said. “Antibiotic resistance is going to happen. We need to get ahead of it and design inhibitors now to protect our antibiotics, because if we wait until it becomes a crisis, it’s too late.”